High Court Malaya, Johor Bahru
Ahmad Kamal Md Shahid J
[Suit No: JA-21NCVC-17-12-2016]
30 March 2023
Tort: Negligence - Medical negligence - Duty of care - Plaintiff suffered irreversible brain damage consequent to treatment and management by defendants - Whether defendants committed various acts of negligence in treatment and management of plaintiff - Whether defendants' negligence materially contributed to plaintiff's injuries - Whether defendants' liable for injury suffered - Quantum of damages to be awarded
This was the plaintiff's claim in medical negligence and/or breach of contract against the defendants for injuries and losses suffered as a result of the medical treatment and management of the plaintiff by the defendants. The plaintiff was admitted to the Hospital owned and managed by the 17th defendant at about 33 weeks of gestation with a diagnosis of type Ill placenta praevia, making the plaintiff a high-risk obstetric case and underwent an emergency Caesarean section for the delivery of her baby. The plaintiff later collapsed and was resuscitated and transferred to the Intensive Care Unit (ICU) of the Hospital. Despite being seen as an inpatient and outpatient at the Hospital and other hospitals; the plaintiff suffered severe and irreversible brain damage. The plaintiff suing through her husband and litigation representative, claimed that the plaintiff's condition was caused or materially contributed by the negligence and breach of contract of the defendants. Accordingly, the main issue to be determined was, whether the defendants had breached that duty of care / standard of care and whether such breach had caused damage and injuries as alleged by the plaintiff.
Held (allowing the plaintiff's claim with costs):
(1) From the evidence adduced, it was clear that the defendants had failed to act on obvious facts without delay with the result that the plaintiff suffered oxygen deprivation leading to serious brain damage. Especially in the ICU, it was not enough to throw oxygen and blood at the plaintiff. Her condition had to be monitored closely. Each material change in her condition had to be acted upon without delay. However, the defendants failed to do so. They allowed her condition to happen and failed to act without delay upon ominous signs such as biting of the ETT by the plaintiff; oxygen desaturation; and high lactate acidosis levels showing a chronic lack of oxygen. Consequently, the defendants had committed various acts of negligence in this case. (paras 97-99)
(2) In the instant case, the multi-disciplinary team consisting of the obstetric team and the anaesthetic & ICU team, had failed in its duties to adequately monitor the plaintiff's condition and therefore its members had to collectively accept responsibility for their failure. From the evidence produced in Court, it was clear that there was an indivisible injury in this case: severe brain damage. Here, the defendants' negligence had materially contributed to the damage suffered by the plaintiff, and thus causation was proven to the extent of 100%. (paras 102, 107, 108 & 110)
(3) In light of the findings in this case, the Court was satisfied that the defendants were liable for the severe brain damage as a result of severe bleeding and lack of oxygen supply to the brain of the patient following a Caesarean section performed upon her in the hospital. In addition, the 17th defendant, the Government, was directly liable both in tort and contract for organisational and system failures and also where it was under a non-delegable duty of care as a provider of healthcare. Thus, the plaintiff had proved its case against the defendants on a balance of probabilities. (paras 146-148)
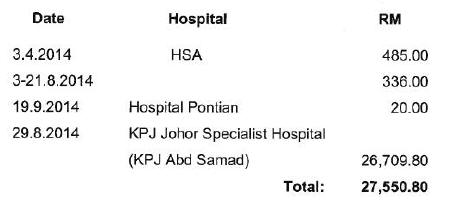
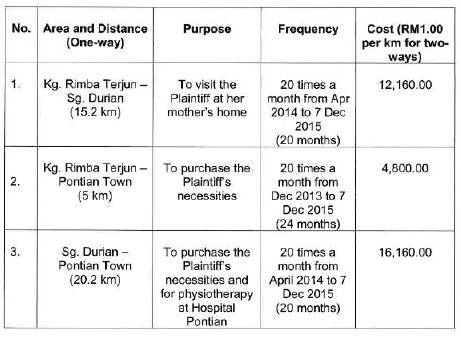
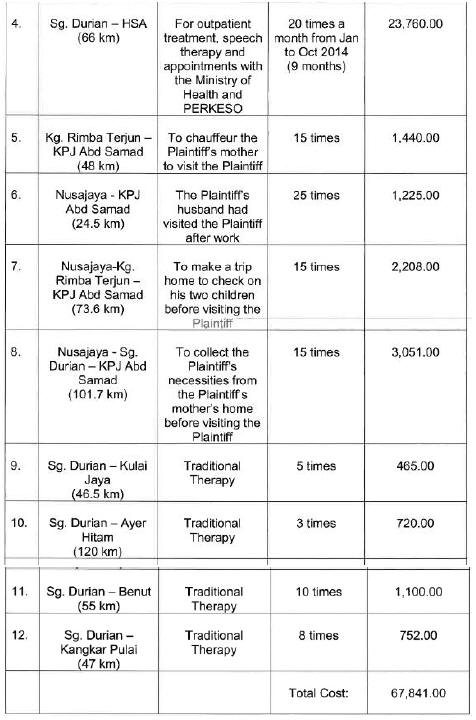
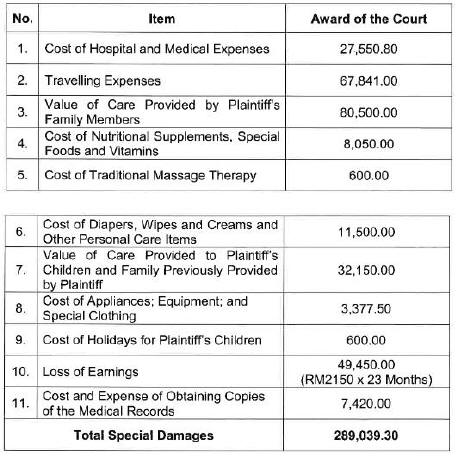
(4) The plaintiff's husband had given evidence regarding the difficulties that he had faced in finding out if the plaintiff had a cause of action and also in keeping copies of all bills and receipts. In this case, as a result of the negligence of the defendants, the plaintiff incurred hospital and medical expenses. Even though the plaintiff's husband could not retain copies of all the bills and receipts for expenses incurred, this should not be a bar to the plaintiff recovering the sums incurred as pleaded under special damages. (Nurul Husma Muhammad Hafiz & Anor v. Kerajaan Malaysia & Ors and Rohgetana Mayathevan v. Dr Navin Kumar & Ors and Other Appeals). (paras 160, 161, 163 & 167)
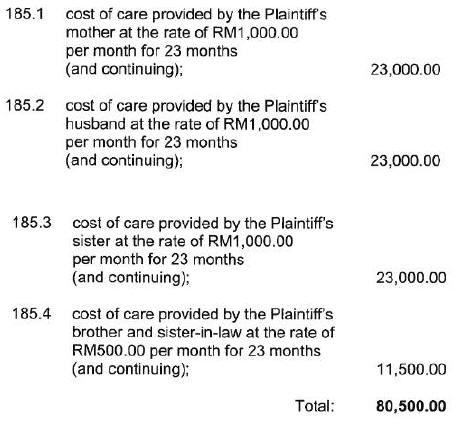
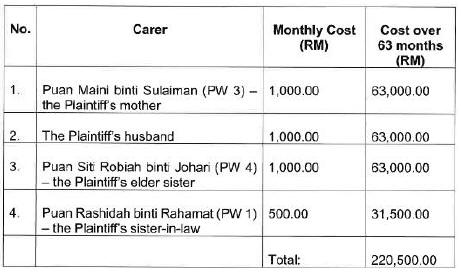
(5) Looking at the injuries suffered by the plaintiff, the plaintiff's family members had made commendable efforts to improve her quality of life. Caring for the plaintiff was no easy chore. It was laborious and taxing. Therefore, it was just and fair that the value of the care given to the plaintiff by the family members must be paid for by the tortfeasors. It was not right to say that, as a family, the plaintiff's relatives had an obligation to care for her. The value of such care does attract an award of damages. Considering the amount of effort and time that all of the family members had invested in caring for the plaintiff, the sum of RM1,000.00 per month was fair and reasonable to be awarded as the cost of care provided to the plaintiff each by her mother, elder sister and husband and RM500.00 per month to the plaintiff's brother and sister in law. (Tan Cheong Poh & Anor v. Teoh Ah Keow). (paras 181-184)
(6) A successful litigant was entitled to the costs of the pre-action discovery proceedings. The access to the records was a necessary step to take before bringing a claim of medical negligence. The plaintiff, his medico-legal advisers; and his experts would not have been able to give advice or opinion on the merits of this action without first having to study copies of the medical records. Therefore, the plaintiff's claim for costs of obtaining copies of medical records was allowed. (paras 211-214)
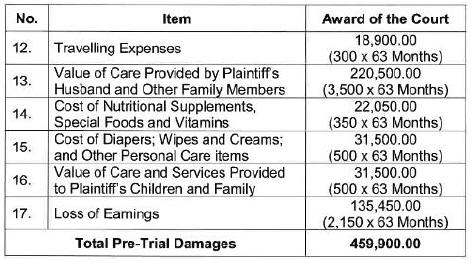
(7) Based on the injuries suffered by the plaintiff, she continued to receive care from her husband, her elderly mother, her elder sister and in-laws. Hence, the pleaded sums for the cost of care for the special damages period should also be awarded for the pre-trial damages period. (paras 220-221)
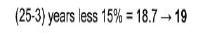
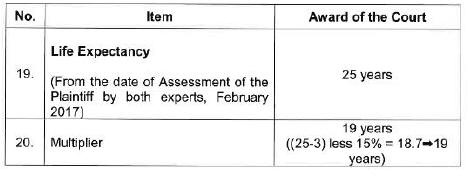
(8) Based on the test as set out by the Federal Court in lnas Faiqah Mohd Helmi v. Kerajaan Malaysia & Ors and the once-and-for-all basis of deciding on life expectancy, the court should err on the side of awarding more instead of less. This was because if the court erred on the side of awarding less, that would result in the plaintiff being out-of-pocket if she survived longer than the life expectancy estimated by the court. In the circumstances of this case, the plaintiff should be given the benefit of the doubt and the life expectancy should be given as 25 years, taking the 22 years estimated by both experts for the plaintiff and the defendant, with an additional three years on account of favorable economics. (paras 258, 259 & 263)
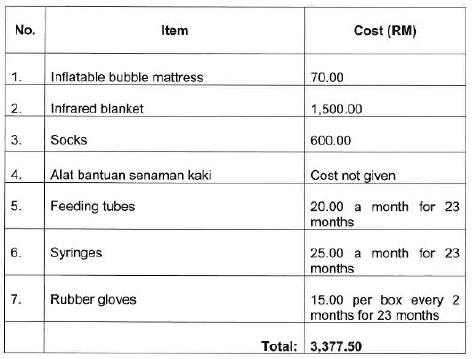
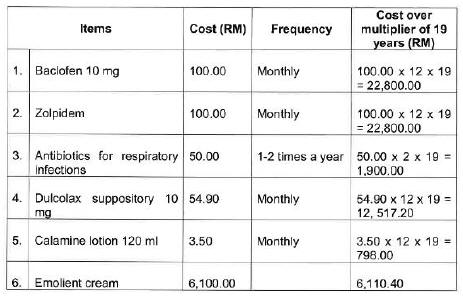
(9) In awarding future needs, the therapeutic benefits of their respective recommendations should be the main consideration when awarding the cost of purchasing such equipment. Given the plaintiff's debilitating condition, the plaintiff should be given every reasonable advantage possible. It would be an 'unjustifiable gamble' for the plaintiff to not be awarded the cost of such equipment, medicine and therapies. (paras 268-269)
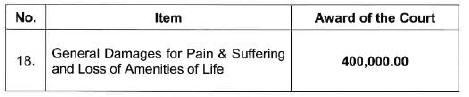
(10) Unlike infants who suffer brain damage at birth, the plaintiff herein had had an appreciation of the joys of life, childhood, marriage, motherhood, successful vocation and etc. The negligence of the defendants had deprived her of all these joys. Her loss of amenities of life was therefore far more than infants who had suffered brain damage at birth. In the circumstances, a sum of RM400,000.00 under the head of damages for pain and suffering and loss of amenities of life was awarded. (paras 316-317)
(11) It was a well-recognised fact that medical negligence litigation was very expensive and medical negligence litigation was difficult, complex, time-consuming and often involved novel questions of law and fact. Going by the complexity and novelty of the issues involved, a sum of RM250,000.00 should be awarded as the getting-up fee for the liability and quantum proceedings. (Farah Ahmed Naji Al Sahhab v. Dr Lee Weng Seng & Ors). (paras 318-327)
Case(s) referred to:
Batu Kemas Industry Sdn Bhd v. Kerajaan Malaysia & Tenaga Malaysia Bhd [2016] 1 MLRA 36 (refd)
Bolam v. Friern Hospital Management Committee [1957] 2 All ER 118 (refd)
Bolitho v. City and Hackney Health Authority [1997] 3 WLR 1151 (refd)
Datuk Mohd Ali Hj Abdul Majid & Anor v. Public Bank Berhad [2014] 4 MLRA 397 (refd)
Dr Premitha Damodaran v. Gurisha Taranjeet Kaur & Anor And Another Appeal [2022] 2 MLRA 502 (refd)
Farah Ahmed Naji Al Sahhaf v. Dr Lee Weng Seng & Ors [2017] MLRHU 1761 (refd)
Fareed Reezal Arund (Mendakwa Melalui Isteri Dan Wakil Litigasinya, Wan Zafura bt Wan Kassim) lwn. Pantai Medical Centre Sdn Bhd dan Yang Lain (KL High Court Suit No WA-22NCVC-33-01/2016) (unreported) (refd)
Foo Fio Na v. Dr Soo Fook Mun & Anor [2006] 2 MLRA 410 (refd)
Hawkins v. New Mendip Engineering Ltd [1966] 3 AUER 228 (refd)
Inas Faiqah Mohd Helmi v. Kerajaan Malaysia & Ors [2016] 1 MLRA 647 (refd)
James Robshaw (A Child by His Mother and Litigation Friend, Suzanne Adams [2015] Med LR; [2015] EWHC 923(QB) (refd)
Nurul Husma Muhammad Hafiz & Anor v. Kerajaan Malaysia & Ors [2015] 1 MLRH 234 (refd)
Piona Abdul Latif v. Kerajaan Malaysia & Ors [2018] MLRHU 527 (refd)
Rogers v. Whitaker [1992] 175 CLR 479 (refd)
Rohgetana Mayathevan v. Dr Navin Kumar & Ors And Other Appeals [2017] 3 MLRA 53 (refd)
Shalini Kanagaratnam v. Pusat Perubatan Universiti Malaya & Anor [2016] 5 MLRA 67 (refd)
Tan Cheong Poh & Anor v. Teoh Ah Keow [1995] 2 MLRA 379 (refd)
Tenaga Nasional Berhad (Formerly Lembaga Letrik Negara Tanah Melayu) v. Perwaja Steel Sdn Bhd (Formerly Perwaja Terengganu Sdn Bhd) [1995] 5 MLRH 406 (refd)
Maria Freeman v. Christopher Lockett [2006] Lloyd's Law Reports (Medical) 151 (refd)
Zulhasnimar Hassan Basri & Anor v. Dr Kuppu Velumani P & Ors [2017] 5 MLRA 399 (refd)
Legislation referred to:
Civil Law Act 1956, s 28
Other(s) referred to:
Alec Samuel The English Tort System for Medical Mishaps', Medico-Legal Journal, 4th edn 2004, vol 72, p 147
Charles J Lewis Medical Negligence - A Plantiff's Guide, 2nd edn, p 39
Powers and Harris Clinical Negligence, 4th edn, para 11.4
Counsel:
For the plaintiff: PS Ranjan (Karthi Kantabalan & Evan Lee Sian Wen with him); M/s PS Ranjan & Co
For the defendants: Nik Mohd Noor Nik Kar (Azlan Bohari, Mohd Khairi Mohd Said & Adiba Iman Md Hassan with him); Attorney General's Office
JUDGMENT
Ahmad Kamal Md Said J:
Introduction
[1] The plaintiff's claim is in medical negligence and/or breach of contract against the Defendants for injuries and losses suffered as a result of the treatment and management of the plaintiff by the Defendants.
[2] The plaintiff claims general damages, special damages, interest and costs in respect of the injuries and losses suffered.
[3] After the hearing, I allowed the plaintiff's claim. This judgment contains the full reasons for my decision.
Background Facts
[4] The background facts as set out in the Statement of Claim are as follows:
4.1 The plaintiff at the material time was 33 years old, suffers from serious and irreversible brain damage rendering her of unsound mind, and brings this claim by her husband and litigation representative Khairil Faiz bin Rahamat;
4.2 The plaintiff and her husband were married on 10 October 2010 and have 2 children, one born on 23 November 2011 and the other on 12 December 2013;
4.3 At all material times the plaintiff was working as an administrative clerk in a company called "Muda Jaya Corporation Sdn Bhd";
4.4 The 1st to 16th defendants are the doctors and nurses who had attended to the plaintiff in Hospital Sultanah Aminah Johor Bahru, (the Hospital) and which is owned and managed by the 17th defendant;
4.5 The 1st to 16th defendants are the servants and agents of the 17th defendant at the Hospital;
4.6 The plaintiff was admitted to the Hospital on 11 November 2013 at about 33 weeks of gestation with a diagnosis of type III placenta praevia, making the plaintiff a high-risk obstetric case;
4.7 On 12 December 2013, the plaintiff underwent an emergency Caesarean section for the delivery of her baby;
4.8 Later, the plaintiff collapsed and was resuscitated and later transferred to the Intensive Care Unit (ICU) of the Hospital;
4.9 The plaintiff was later seen as an inpatient and outpatient at the Hospital and other hospitals;
4.10 The plaintiff suffered severe and irreversible brain damage which was caused or materially contributed by the negligence and breach of contract of the defendants and each of them;
4.11 The 17th Defendant as the owner and manager of the Hospitals and as the employer of the 1st to 16th Defendants is vicariously liable for the negligence of the 1st to 16th Defendants;
4.12 The plaintiff avers that the 17th Defendant also owed to the plaintiff a non-delegable duty of care for the plaintiff's safety and also owed a non-delegable duty of care to avoid organizational and system failures;
4.13 The plaintiff avers that the Defendants and each of them owed to the Plaintiff a duty in contract and the law of due care and skill, diligence, candour and good faith, and to act in the best interests of the Plaintiff; and
4.14 The plaintiff's claim against the Defendants and each of them is for negligence and breach of contractual and other duties in regard to the management of her condition which negligence and breaches of duties caused or materially contributed to the personal injury and loss and damage suffered by the plaintiff.
The Plaintiff's Case
[5] The plaintiff's claim is in medical negligence and/or breach of contract against the Defendants for injuries and losses suffered as a result of the treatment and management of the plaintiff by the Defendants.
[6] In gist, the plaintiff's case is as follows:
6.1 she was referred to the Hospital at 33 weeks gestation with expectant management of Placenta Previa Type 3 posterior;
6.2 the plaintiff was a high-risk obstetric case;
6.3 on 12 December 2013, she delivered her baby by emergency Caesarean section;
6.4 immediately after delivery she was noted to have lost around 300 ml of blood;
6.5 she then collapsed and cardiopulmonary resuscitation was undertaken for 5 minutes after which she recovered;
6.6 the impression was "amniotic fluid embolism with DIVC";
6.7 at the end of the operation there were three figures given as the total estimated blood loss which were 1.5, 2.0 and 2.5 liters;
(See: 1. the Integrated Notes on p 161 of Bundle A1;
2. the Operation Record on p 166 of Bundle A1; and
3. Dr Lum's (PW 7) reference to the Complaint's Investigation Report in para 23 of his expert report on p 56 of the Bundle of Experts' Reports marked as Bundle C);
6.8 despite obtained from the resuscitation in the operation theatre, it was lost quickly because the management while she awaited transfer to the ICU and also the management in the ICU was below accepted standards;
6.9 the further bleeding contributed to another bout of lactic acidosis which was reflected in the high lactate levels, meaning that there was oxygen deprivation;
6.10 the plaintiff was left in a chronic hypoxic state, as shown by high lactate acidosis levels, for about 21 hours which led to brain damage;
6.11 the accepted standards of cerebral protection required the plaintiff's temperature to be brought down to normothermia, between 36°C and 37°C (a lower temperature would reduce the brain's need for oxygen);
6.12 the temperature was well over normothermia several times and was never brought down to normothermia during the material period;
6.13 the specialist who was in charge Dr Nor'Azim (DW 5) gave evidence but the nurses who were attending to the plaintiff in the ICU did not; and
6.14 Dr Nor'Azim did not write any contemporaneous notes at all.
[7] The plaintiff has suffered severe and irreversible brain damage with severe permanent physical and mental disabilities.
[8] The principal thrust of the plaintiff's allegations against the 1st to 16th defendants are as follows:
8.1 failed to act in accordance with their statutory duties under the law;
8.2 performed unnecessary medical procedures and undertook medical procedures in the wrong manner;
8.3 caused the plaintiff to suffer various injuries when undertaking the medical procedures;
8.4 that there was a failure to undertake close monitoring of the plaintiff following her collapse in the operation theatre;
8.5 that there was a failure to properly estimate the amount of bleeding suffered by the plaintiff;
8.6 that there was a failure to undertake proper transfusion of blood and volume replacement for the plaintiff;
8.7 that there was a failure to properly treat the plaintiff's metabolic abnormalities;
8.8 that there was a failure to undertake proper cerebral protection measures for the plaintiff;
8.9 that the plaintiff and her husband were given insufficient advice and information; and
8.10 that the Defendants had failed to have a proper and adequate system for multidisciplinary consultations, discussion, treatment and management of the plaintiff's condition.
[9] The principal thrust of the plaintiff's allegations against the 17th Defendant are as follows:
9.1 failed to have in place or follow proper and effective systems in providing healthcare services to the plaintiff, in failing to engage healthcare practitioners with sufficient qualifications and experience, in failing to provide sufficient facilities for the proper and effective management of patients such as the plaintiff, in failing to inform the plaintiff of treatment options elsewhere for better management of her condition, an in failing to act in accordance with its statutory duties under the law.
[10] The plaintiff claims general damages, special damages, interest and costs in respect of the injuries and losses suffered.
The Defendants' Case
[11] The plaintiff was pregnant with her second child in 2013. She was referred to the Hospital from Klinik Kesihatan on 11 November 2013 for Placenta Praevia Type III Posterior. She had no prior history of antepartum haemorrhage. She was scheduled for an elective Caesarean Section at 38 weeks period of amenorrhoea on 16 December 2013. She continued to be admitted to the ward for rest and monitoring.
[12] On 12 December 2013, the plaintiff started to have contraction pain and an emergency Caesarean Section was planned on the same day. The operation started at 11.05 am under general anaesthesia. A baby boy was delivered at 11.17 am weighing 3.1kg.
[13] Soon after delivery of the baby, the plaintiff became bradycardic with a heart rate of 40 bpm. Oxygen saturation and capnograph were not recordable. The patient subsequently developed Pulseless Electrical Activity. CPR was immediately commenced. After 5 minutes of resuscitation there was a return of spontaneous circulation with the pulse rate of 145 and blood pressure of 110/70. A diagnosis of Amniotic Fluid Embolism (AFE) was made.
[14] The plaintiff subsequently developed bleeding from the vagina and puncture sites. Uterus was not well contracted. IV Oxytocin 80 units infusion, 4 doses of IM carboprost and the continuous uterine massage was administered. The estimated blood loss was 2L. She was transfused 2 pints of packed cells (PC), 6 units of cryoprecipitate (Cryo), 4 units of platelets, 2 units of fresh frozen plasma (FFP), cystalloids and colloids. IV Adrenaline was also initiated to support her haemodynamics at 1 mcg/kg/min. The patient had developed Primary Post-partum Haemorrhage with Disseminated Intravascular Coagulopathy. The surgery lasted for about 2 hours. The care of the patient in the operating room was provided by a specialist and a medical officer (MO) of the obstetric department and similarly, one specialist and one MO of the anaesthesia team.
[15] The plaintiff was then transferred to ICU for further management and stabilization. Arterial Blood Gas (ABG) in the ICU at 2.30 pm showed metabolic acidosis, pH 7.137 and lactate was 6.0 mmol/L. Hb was 10.4 g/ dL. She was kept sedated. Further transfused another 4 units of packed cells, 12 units of cryo, 8 units of platelets and 4 units of FFP. She responded with these therapies as the inotropes were tapered down and acidosis improved. A repeat ABG at 4.00 pm showed her lactate level decreased to 4.6 mmol/L. pH was 7.23, Hb was 10.9 g/dL. Initial ventilator settings were Assist control/ volume control (ACVC), Fi2 of 1.0 with a Positive End Expiratory Pressure (PEEP) of 10-12 cmH20. The Fi02 was subsequently tapered down to 0.4 and PEEP was maintained at 10 cmH20 in relation to the improvement in the Pa02 from the ABG. Her temperature was noted to be in the range of 35.9°C-37.7°C for the first 6 hours. Later on, the plaintiff was febrile with a temperature of 38.2°C-39.0°C, which resolved on Post-operative day (POD) 2 with tepid sponging. PEEP was further winded down to 8 cm H20 from POD 2.
[16] On POD 1, in view of poor Glasgow Coma Scale (GCS) recovery, plain CT brain was done on 15 December 2013 (POD 3) about 3 days after the cardiac arrest. The scan revealed no intracranial bleed, white and grey matter was well differentiated. Ventricles, basal cisterns and sulci were preserved. No evidence of ischaemia. Despite that the husband was explained that the poor GCS recovery may be due to brain ischaemia following the cardiac arrest.
[17] POD 3, the plaintiff started to have a spiking temperature. Septic workout was done and she was started on IV Imipenem.
[18] As, GCS remained the same until 17 December 2013, a CT contrast was performed. There was poor white and grey matter differentiation with a more hypodense area at both thalamic regions compared to the previous CT scan. Ventricles, basal cisterns and sulci were still preserved. This was suggestive of underlying oedema or Hypoxic Ischaemic Encephalopathy (HIE).
[19] Tracheostomy was performed on 20 December 2013 by the surgical team without any complication.
[20] It was noted in the notes, that the husband was kept updated on her progress and understood what was being explained.
[21] On 21 December 2013, the plaintiff was able to be taken off from the ventilator. She was put on trachemask with 2 of 6 L/m. GCS showed some improvement to 10/15 (E4VTM5).
[22] She was discharged from the ICU on 26 December 2013. The husband was told that the poor GCS is secondary to HIE following amniotic fluid embolism, sepsis was being treated with antibiotics and she would require nursing care.
[23] The plaintiff was eventually referred to Rehabilitory Physician for rehabilitation which included physiotherapy, occupational and speech therapy. She was also referred to Jabatan Kerja Sosial Perubatan for support. All of these were done to aid the patient and family for her care when she is discharged home.
[24] The plaintiff was discharged home on 3 April 2014. Upon discharge, she was able to speak a few words, understand simple commands. However, she was still ADL (activity of daily living) dependant. She was given follow-up to a rehabilitation clinic.
[25] The defendants had done their level best to treat the plaintiff. It was unfortunate that the effect of Amniotic Fluid Embolism had caused the plaintiff to suffer a permanent neurological deficit.
Trial
[26] The trial of this suit took 23 non-consecutive days. In the course of the trial, the parties called the following witnesses respectively whom all gave sworn testimonies.
[27] The plaintiff's witnesses were:
27.1 her sister-in-law Puan Rashidah binti Rahamat (PW 1);
27.2 her mother-in-law Puan Saleha bt Hamdan (PW 2);
27.3 her mother Puan Maini binti Suliman (PW 3);
27.4 her elder sister Puan Siti Robiah binti Johari (PW 4);
27.5 her husband and litigation representative Encik Khairil Faiz bin Rahamat (PW 5);
27.6 her expert on liability consultant anaesthesiologist Professor Dr Chan Yoo Kuen of the University of Malaya Medical Centre (PW 6);
27.7 her expert on liability consultant obstetrician and gynaecologist Dr Milton Lum Siew Wah of Alpha Specialist Centre (PW 7); and
27.8 her expert on quantum consultant rehabilitation physician Professor Dr Lydia binti Abdul Latif of UM Specialist Centre (PW 8).
[28] The defendants' witnesses were:
28.1 their expert on quantum consultant rehabilitation physician Dr Akmal Hafizah binti Zamli of the Sungai Buloh Hospital (DW 1);
28.2 the 2nd Defendant Dr Senthi s/o N. Muthuraman (DW 2);
28.3 the 9th Defendant Dr Shazlina Shirin bt Jamaludin (DW 3);
28.4 the 10th Defendant Dr Adlina bt Hisyamuddin (DW 4);
28.5 the sessional intensivist Professor Dr Nor'Azim Mohd Yunos (DW 5); and
28.6 their expert on liability consultant anaesthesiologist Dr Mohd Rohisham bin Zainal Abidin of the Tengku Ampuan Rahimah Hospital, Klang (DW 6).
The Burden Of Proof
[29] It is well settled that the onus lies on the plaintiff to prove the elements of negligence in order to succeed in his claim against the Defendants pursuant to ss 11 and 102 of the Evidence Act 1950. [See the cases of Datuk Mohd Ali Hj Abdul Majid & Anor v. Public Bank Berhad [2014] 4 MLRA 397 and Tenaga Nasional Berhad (Formerly Lembaga Letrik Negara Tanah Melayu) v. Perwaja Steel Sdn Bhd (Formerly Perwaja Terengganu Sdn Bhd) [1995] 3 MLRH 196; [1995] 5 MLRH 406].
[30] In the case of Shalini Kanagaratnam v. Pusat Perubatan Universiti Malaya & Anor [2016] 5 MLRA 67 the Court of Appeal enunciated the four (4) elements that a plaintiff has to prove in cases of medical negligence as follows:
"[9] In cases of professional negligence and/or medical negligence, the plaintiff has to prove four elements. They are: (i) duty of care; (ii) breach of standard of care; (iii) breach of duty of care; (iv) caused damages. In consequence, the plaintiff has to lead evidence to show the standard of care has been breached. The doctrine of r es ipsa loquitur will not ordinarily apply as the plaintiff will have to discharge the legal burden and only after the legal burden has been discharged, the defendant has to satisfy that legal duty was not breached".
[31] Reference is also made to the case of Muthu Subramaniam v. Dr Wan Hazmy Che Hon [2018] MLRHU 1291 where Abu Bakar Jais J (now JCA) held that the burden to prove negligence lies on the plaintiff and it is not the obligation of the defendant to disprove the allegations of negligence in the Statement of Claim and it was held as follows:
"[34] It is trite that the burden of proof in cases of medical negligence such as this is on the plaintiff. It is the plaintiff's burden to prove negligence against the FD on the basis that what was done was what a reasonably competent practitioner skilled in that particular act would or would not have done. The FD has no obligation to disprove the allegations of negligence in the statement of claim. (See the cases Wu Siew Wong v. Pulau Pinang Clinic Sdn Bhd & Anor [2010] 1 MLRH 956 Mathew Scott Oakley & 2 Ors v. Dr George Varugese & Anor [2009] 5 MLRH 93; [2010] 10 CLJ 322 and Payremalu Veerappan v. Dr Amarjeet Kaur & Ors [2001] 2 MLRH 101)".
[Emphasis Added]
[32] Applying the abovementioned, the onus lies on the plaintiff to prove negligence on a balance of probabilities and in particular the following elements:
(a) that there was a duty of care owed by the Defendants;
(b) that there was a breach of the standard of care by the Defendants;
(c) there was a breach of the duty of care by the Defendants; and
(d) that the said breaches have caused damage to the plaintiff.
Standard Of Care Expected Of The Defendants
[33] The law in relation to the standard of care in medical negligence cases appears to now be settled as enunciated in the Federal Court case of Zulhasnimar Hassan Basri & Anor v. Dr Kuppu Velumani P & Ors [2017] 5 MLRA 399 where it was held as follows:
"[94] Thus, it is our judgment that in respect of the standard of care in medical negligence cases, a distinction must be made between diagnosis and treatment on the one hand and the duty to advise of risks on the other. This is because diagnosis and treatment are purely in the realm of medicine and that in the field of medicine, there are genuine differences of professional opinion in respect of diagnosis and treatment. Although as a discipline, medicine involves specific knowledge, its practice, however, often does not admit to scientific precision. It is not always the case that there is a definite answers one way or the other. In fact, medical experts do genuinely and frequently differ in opinion on diagnosis and treatment.
[95] Given the fact there are genuine differences in opinion in diagnosis and treatment, it is therefore not a matter that the Court can, or is, equipped to resolve. It is in this context that the Bolam test makes good sense. It requires the Court to accept, not just the views of medical experts simpliciter, but the views of a responsible body of men skilled in that particular discipline. It removes from the Courts the responsibility of resolving a dispute that is not equipped to resolve.
[96] On the other hand, different consideration ought to apply to the duty to advise of risks as opposed to diagnosis and treatment. That duty is said to be noted in the right of self-determination. As decided by the Australian High Court in Rogers v. Whitaker and followed by this Court in Foo Fio Na, it is now the Courts' (rather than a body of respected medical practitioners) which will decide whether a patient has been properly advised of the risks associated with a proposed treatment. The Courts would no longer look to what a body of respectable members of the medical profession would do as the yardstick to govern the standard of care expected in respect of the duty to advise".
[34] The historical development of the law relating to medical negligence was also discussed extensively in the recent Court of Appeal case of Dr Premitha Damodaran v. Gurisha Taranjeet Kaur & Anor And Another Appeal [2022] 2 MLRA 502 where after undertaking the exercise of referring to various decided cases including Bolam v. Friern Hospital Management Committee [1957] 2 All ER 118; Rogers v. Whitaker [1992] 175 CLR 479, HC; Bolitho v. City and Hackney Health Authority [1997] 3 WLR 1151; and the Federal Court case of Foo Fio Na v. Dr Soo Fook Mun & Anor [2006] 2 MLRA 410, the Court of Appeal concluded as follows:
"[23] This anomalous situation was put to rest by the Federal Court in Zulhasnimar Hassan Basri & Anor v. Dr Kuppu Velumani P & Ors [2017] 5 MLRA 399 where it was held that the test in Rogers v. Whitaker; followed by Foo Fio Na, in regard to the standard of care in medical negligence is restricted only to the duty to advise the risks associated with any proposed treatment and does not extend to diagnosis or treatment. With regard to the standard of care for diagnosis or treatment, the Bolam test still applied, subject to the qualifications in Bolitho. The Federal Court was of the view that in 'respect of the standard of care in medical negligence cases, a distinction must be made between diagnosis and treatment on the one hand and the duty to advise of risks on the other. This is because diagnosis and treatment are purely in the realm of medicine and in the field of medicine, there are genuine differences of professional opinion in respect of diagnosis treatment.
[24] With that, the law as to the standard of care in medical negligence cases in Malaysia was well settled...."
The Decision Of The Court
Liability
[35] The central issue in this case is whether the Defendants had breached that duty of care / standard of care and whether such breach had caused damage / injuries as alleged by the plaintiff.
Various Possible Acts Of Negligence Alleged By The Plaintiff
[36] The burden lies on the plaintiff to prove that the Defendants or any of the Defendants had committed the act of negligence. It must also be proven by the plaintiff the causation link between the act of negligence and the injuries suffered by the plaintiff.
Inadequate Documentation And Underestimation Of Blood Loss
[37] It is important to make accurate records of the diagnosis, treatment and plan of a patient in the medical records. This was admitted by Dr Senthi (DW 2) during cross-examination (See: page 1058 of the Notes of Evidence (NOE)).
[38] Having perused the relevant Bundle of Documents, I find that there were inadequate documents with regard to the blood loss and monitoring of the plaintiff's vital sign. Such lapses obviously had an adverse effect on the condition of the plaintiff.
(See: paragraphs 124 and 125 of Dr Lum's Expert Report on p 69 of Bundle C)
[39] Further, I noticed that there were no monitoring records during the period between 1.00 pm and when the plaintiff was transferred to the ICU at about 2.25pm.
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1718 of the NOE)
[40] The evidence of Dr Milton Lum Siew Wah (PW 7) shows that there were inconsistencies in the amount of the plaintiff's estimated blood loss and the actual number of units of blood that were transfused. The blood loss at one stage was estimated to be as low as 1,500 ml by one practitioner and 2.500 ml by another. It also showed inadequate monitoring of the plaintiffs condition and the amount of blood loss was likely higher than 2.5 liters.
(See: Examination in Chief of Dr Milton Lum (PW 7) on pp 481 and 482 of the NOE; Re-Examination of Dr Milton Lum (PW 7) on pp 563 and 564 of the NOE; Intensive Care Chart for 12 December 2013 on p 15 of the Bundle L)
[41] This fact was admitted by the Defendants' witness, Dr Senthi (DW 2) when he said that there were omissions in the medical records and nothing was done to correct the discrepancies.
(See: Cross-Examination of Dr Senthi (DW 2) on pp 898, 899, 92 and 903 of the NOE)
[42] Further, the evidence from the witnesses clearly shows that the danger that arose in this case was underestimating of the blood loss and therefore inadequate and untimely transfusion of blood.
[43] This can be seen from the evidence of Dr Milton Lum (PW 7) when he said as follows:
(i) "A This p 873 is for the date 26 December 2013, which is way after the event when the patient collapsed. But normally when a patient collapses and we resuscitate the patient, one of the charts that we do is to put in an Intake/Output Chart, so everybody knows how much has been given to the patient, everybody knows how much has been lost.
Q: How important is it, in the OT itself?
A: This Intake/Output Chart guides us in replacing the fluids, the blood that the patient had lost and it allows communication between doctors and nurses. So, everybody knows exactly how much has been lost or estimated to be lost and everybody knows how much blood or other fluids or drugs that have been given to the patient. Apart from that, we also record the patient's vital signs, the blood pressure, the pulse, the temperature etc. I do not find those records in the immediate period after the patient collapsed, there was some anaesthetic records but the anaesthetic records from the Anaesthetist lasted only 2 hours. The anaesthetic records are found in p 702 of Bundle A3.
Q: From what time was the anaesthetic record commenced?
A: If you look at the at the end of the first third of the chart, right at the top, after 12 December 2013, next to it is 1100 hours. So, the anaesthetic record commenced at about 11.00 am and there was recording until the end of the second third of the chart, which was about 2 hours later because if you look at the chart, it measures in 00,10, 20, 30, 40, 50, 60, 00, that is in minutes. So, if you look at this, the anaesthetic record lasted about 2 hours because it went to 00 two times. So, you can interpret from here that the record was from 11 o'clock to about 1 o'clock, about 2 hours, thereabouts. But the patient was still in the OT and was only transferred to the ICU or reached the ICU at 2.25 pm. So, there is practically no record of the patient's vital signs from about 1.00pm till 2.25 pm, time period of 1½ hours.
Q: In a case like this, would you accept this non-recording?
A: I don't think it's acceptable at all.
Q: Why?
A: Because when you resuscitate a patient, you have to have all the information you need to resuscitate the patient. You got to know whether your resuscitation efforts are sufficient for the patient, you got to know whether the amount of blood that you give to the patient is able to compensate the patient at least to some extent for the amount of blood that is lost.
Q: So Doctor, no Intake/Output chart in the OT after she collapsed. Recording between 11.00 pm and 1.00 pm regarding anaesthetic matter, with just this material, in your opinion, could the team have managed the post-resuscitation period properly?
A: It would have been very, very difficult because there is not just one person managing the resuscitation of this patient, there are doctors involved, there are nurses involved. The doctors are obstetricians, the doctors are anaesthetists, the nurses, they change their shift, so it's important that we have records so that everybody is on the same page and you know exactly how much was given, fluids-wise, blood and blood products and you know how much blood was lost. You also want to know what the patient's vital signs are. The patient's vital signs are in this bottom half here, the blood pressure and the pulse of p 702, they are there. But they stop at about 1.00pm, we don't know what happened from 1.00 pm to 2.25 pm."
[Emphasis Added]
(See: Examination in Chief of Dr Milton Lum (PW 7) on pp 483 to 486 of the NOE)
(ii) Dr Shazlina Shirin bt Jamaludin (DW 3) in her evidence had stated as follows:
"Q: Doctor, if blood loss is under-estimated, that can mean harm for the patient?
A: Betul
Q: And if it is over-estimated??
A: Also will be harmful
Q: Why?
A: Jika darah berlebihan, ada komplikasi dengan blood transfusion yang kelebihan kepada pesakit juga
Q: So excessive blood transfusion can harm a patient, correct?
A: Ya
Q: So, as a general principle, that when you are managing massive blood loss, it is important to estimate as accurately as possible the blood loss and also it is important to give a proper amount of blood and blood products for the patient, correct Doctor?
A: Betul"
(See Cross-Examination of Dr Shazlina (DW 3) on pp 947 and 948 of the NOE)
(iii) Dr Mohd Rohisham (DW 6) in his evidence had stated as follows:
"Q: Doctor, you see, while she was losing blood, it was coming out, blood was being put in but there is no intake and output chart during that period?
A: Yes
Q: Now, Dr Lum's criticism is, before you can start on a compensation plan to replace blood loss, you must first have a reliable estimate of the blood loss, would you agree with him on that point?
A: Yes
Q: Now, after that, then you have to see how much has been given, correct, in terms of blood and blood products?
A: Yes
Q: There is a record in the OT that she was given blood and blood products. So, you must see, what has been put in and what is still being lost. Doctor, if there is no record of what had been lost during that 1 hour and 45 minutes before the patient arrived at the OT (correction, ICU), that is a matter for concern, would you accept that?
A: Yes
Q: So Dr Lum's point is that because of the absence of such information, that would harm the effort at replacing blood loss, that's his point. As an experienced Obstetrician, he says that. Dr Senthi kept arguing. My point is, Doctor, surely it should be a matter for concern that there is no record of blood loss during that critical period of 1 hour and 45 minutes, would you see that?
A: Yes
[Emphasis Added]
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on pages 1530 and 1531 of the NOE)
[44] Therefore, inadequate and untimely transfusion of blood resulted in the reduction of both blood volume + oxygen - carrying capacity which caused brain hypoxia.
(See: paragraphs 90 and 130 of Dr Milton Lum's Expert Report on pp 64 and 70 of Bundle C)
Failing to bring down the temperature to Normal or Below Normal
[45] It is to be noted that one of the aspects of management in the instant case is to bring the temperature down to normal or below normal (anything below 36°C).
[46] Cooling was necessary to reduce the energy demands of the body so as to reduce secondary damage to the brain and with the cooling the need for oxygen would be reduced.
[47] This has been testified by both the plaintiff and the defendants witnesses when they testified as follows:
(i) (See: Examination in Chief of Prof. Dr Chan Yoo Kuen (PW 6) on pp 176 to 178 of the NOE)
"Q: Professor, in a case like this, how necessary was cooling of the brain?
A: Here we have a patient with, in fact, no more reserves. If anything, the reserves are not there anymore of oxygen, of energy in the brain. You can actually help the patient reduce what we call secondary damage, that means the care must be such that, you know, reduce as much damage, we call it damage control, as possible. And one of the damage control strategy is to reduce the energy requirement of the brain by cooling it.
....
Q: Professor, to allow the patient to go to 39°C. what kind of damage can occur?
A: As I mentioned earlier, for every 1° rise in temperature, you need an extra 7% of energy in the whole body. So similarly, the brain's requirement for energy is actually very huge. In a normal person like you and I, it takes up 20% of our daily energy requirement. The brain is only about 1,400gm or 1.4kgs, looks very small in a 70kgs man but the energy requirement to sustain it is 20% of our daily energy requirement. So, you can see that the energy requirement to sustain a normal brain is very high."
[Emphasis Added]
(ii) (See: Cross-Examination of Dr Adlina (DW 4) on page 1009 of the NOE)
"Q: Doctor, the purpose of this active cooling is that it will reduce the energy demands of the body, correct?
A: Ya, betul.
Q: And so when the body is cooled, the energy demands are reduced, the oxygen demands too will be reduced?
A: Ya.
Q: Here is a patient where you fear is not getting enough oxygen into the brain?
A: Ya, betul.
Q: So this active cooling is to protect the brain, correct?
A: Ya, betul.
Q: So the process is, cool the body, less energy used, less demand for oxygen, therefore the brain does not suffer?
A: Ya, betul."
[Emphasis Added]
(iii) (See Cross-Examination of Dr Nor'Azim (DW 5) on pages 1262,135 and 1306 of the NOE)
"Q: Now the plan was that the temperature should come down to 32°C to 34°C?
A: Yes
Q: Because with lower temperature, the brain would use less oxygen?
A: Yes
Q: Why you should have that, a lower body temperature, is so that oxygen demands of the brain would be easier to satisfy, would that be correct?
A: Correct
Q: Now, first of all Doctor, if you look at active cooling, the idea is to bring down the temperature so that the body will need less oxygen?
A: Yes
Q: So, in the ICU, you were concerned about this, that if the patient does not get enough oxygen supplying her tissues, she would suffer harm. You were concerned about that, correct?
A: Yes, we are concerned
Q: Therefore, that you're also concerned that the brain needed protection by way of a lower body temperature
A: Yes
Q: S o Doctor, never mind the range, 36 C to 38 C or my figure of 37 C, the point therefore is, when the temperature is elevated, the more the brain's demand for oxygen?
A: Yes"
[Emphasis Added]
(iv) (See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1625 of the NOE)
"Q: Dr, if you.... In regard to the oxygen needs of the patient, particularly when it comes to the brain, you must accept that the brain's oxygen demands are greater that in the case of other parts of the body. Is that correct?
A: Yes.
Q: Now, and if the brain is cooled, it would require less oxygen.
A: Yes.
[Emphasis Added]
[48] Based on ICU Admission Form on p 163 of Bundle A1, I find that there was a written order on 12 December 2013 (Day No 1) to bring the temperature down to between 32° and 34°C for around 12 hours but as admitted both Dr Shazlina (DW 3) and Dr Adlina (DW 4) that the goal to bring the temperature down was never achieved.
(See: Cross-Examination of Dr Shazlina (DW 3) on page 1010 of the NOE and Dr Adlina (DW 4) on page 1020 of the NOE)
[49] It is to be noted that Dr Shazlina (DW 3) had stated in her witness statement "WSD-3" that active cooling was undertaken using a blower, paracetamol and cool saline. However, upon perusal of the medical record, I find that there was no mention of a blower and cool saline being used. The saline was not described as being cold. There was also no mention of ice cubes being used.
(See: Cross-Examination of Dr Shazlina (DW 3) on page 1001 of the NOE; Cross-Examination of Dr Adlina (DW 4) on pages 1186 and 1187 of the NOE and Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1631 of the NOE)
[50] Dr Shazlina (DW 3) had admitted that paracetamol was not effective in bringing the temperature down to 32°C and 34°C. In fact, I find that the first dose of Paracetamol was given quite late at 12.00 pm on 13 December 2013 (Day No 2), about 22 hours after the plaintiff had arrived in the ICU.
(See: Cross-Examination of Dr Shazlina (DW 3) on page 1006 and page 1016 of the NOE)
[51] Further, I also noticed that there was a failure to follow written instructions for cooling so as to achieve even normothermia. This to me, was an act of negligence sufficient to cause or materially contribute to the brain damage.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1300 of the NOE)
[52] Dr Adlina (DW 4) admitted that Hyperthemia, which is the temperature above the normal level; is the most dangerous type of temperature level because the brain's need for oxygen would then be higher than normal when she said the following:
(See: Cross-Examination of Dr Adlina (DW 4) on page 1021 of the NOE)
"Q: But you did not achieve the goal and you said it is because of her condition. Now, the point is therefore, if the temperature is not brought down, the patient will be in an even worse hypoxic state, correct?
A: Betul"
[Emphasis Added]
[53] Dr Nor'Azim (DW 5), after being referred to medical literature, said that for every 1°C rise in temperature above the normal, the brain's need for oxygen would increase between 7% and 15%.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1313 and 1314 of the NOE)
[54] Dr Adlina (DW 4) had given the range of 36°C and 37°C to be the normal body temperature while Dr Nor'Azim (DW 5) had said that the range of 36°C to 38°C was acceptable to him.
(See: Cross-Examination of Dr Adlina (DW 4) on pages 104 and 1005 of the NOE and Cross-Examination of Dr Nor'Azim (DW 5) on page 1284 of the NOE)
[55] Dr Nor'Azim (DW 5) later agreed that plaintiff's temperature had been above normal for 13 hours between 12.00 am and 1.00pm on 13 December 2013 (Day No 2) and there was hyperthermia during that period and that the team should have been concerned about the temperature being above 37°C for those 12 hours when he said the following:
"Q: Doctor, please look at the ICU charts again for the first and second days. On the first day, at about midnight, the temperature was given as 39°C, can you see that?
A: Yes
Q: Now, the condition of, shall I say hyperthermia, continued until the next day at about 12 noon, correct Doctor?
A: Yes
Q: So, it came down to 37°C about 12 hours later. That is going by your position that normal temperature would be between 36°C and 38°C?
A: Yes
Q: Now, in the first 24 hours, temperature above 37°C during a 12- hour period before the end of that 24-hour period is a significant point, correct?
A: Yes
Q: In fact, the team should be concerned about bad result as a result of that temperature?
A: Yes
[Emphasis Added]
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1332 of the NOE and Intensive Care Charts on 12 December 2013 and 13 December 2013 on pp 14 and 15 of Bundle L)
[56] In fact, during the first 7 days in the ICU, I find that the temperature had frequently been above normal.
(See: pages 8 to 15 of Bundle L; and Table of ABG Trends prepared by Professor Chan on pp 6 to 8 of Bundle D)
[57] The defendants' expert Dr Mohd Rohisham (DW 6) had agreed that the elevated temperatures on 16 December 2013 (Day No 5) were not a good thing for the plaintiff.
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1686 of the NOE)
[58] In addition to that, I find that Dr Nor'Azim (DW 5) had agreed that there is scant information in the medical records as to whether the initial goal of cooling the plaintiff to between 32°C and 34°C was either not achieved or abandoned.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1298 of the NOE)
[59] A second order for active cooling was noted to have been given at or around 12.00pm on 13 December 2013 (Day No 2).
(See: Integrated Notes on p 198 of Bundle A1)
[60] Dr Nor'Azim (DW 5) had testified that the goal was to bring down the temperature to "anything below 36°C". However, that goal was never achieved.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1300 and 1301 of the NOE)
[61] Dr Nor'Azim (DW 5) whilst under cross-examination had in fact agreed and conceded that it was important to manage the high temperature on 12 December 2013 when he said the following:
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1328 to 1331 of the NOE)
A: It is to be treated, infection is to be treated, I agree but it's within a range otherwise the protocol would have told us to cool the temperature for 48 hours. But the protocol, as we could clearly see, is only recommending 12 to 24 hours.
Q: Doctor, whatever the protocol may say, you have to look at the needs of the patient that you're treating?
A: Yes, that's what we're doing
Q: Doctor, would you agree or disagree that I'm saying you're saying these temperatures, in relative terms, are not significant?
A: Yes
Q: I am saying they are significant enough, otherwise you won't be treating them?
A: We are treating the infection that is the underlying cause of the temperature
Q: Doctor, would you accept that your duty is also to reduce temperature while fighting an infection?
A: We don't actively reduce the temperature whenever there's an infection, we don't actively cool a patient when the infection causes the high temperatures, that's not our practice, we treat the infection by finding the source of the infection and by giving appropriate antibiotics
Q: Would it help to bring down the temperature if you can fight the infection?
A: I agree with the fact that the brain needs.... Or high temperature, especially in the initial days, 12 to 24 hours maybe 24 to 48 hours, it is important that we take control of the temperature if we could. But beyond that, the concern is if it is just a one spike of 39.4°C and after that it came down to 38°C, which is an acceptable range, we don't actively treat...
Q: So Doctor, first 48 hours, important about temperature coming down?
A: Yes
Q: Beyond that, it is only less important, is that right?
A: Yes
Q: But you cannot say not important at all?
A: No, otherwise we would not have treated the infection"
[Emphasis Added]
[62] I find that the case notes show that the instructions to undertake body and therefore brain cooling were not followed. Therefore, I am of the view that there was no excuse for not following the instructions which had twice been put in writing.
[63] Further, the fact that the instructions were given for cooling shows that such a procedure, if carried out, was intended to make a material contribution to a good outcome.
[64] Thus, I view that the failure to cool the brain is more than a material contribution to the brain damage.
[65] I view that it was reasonably foreseeable that there would be an insufficient flow of oxygen to meet the extra needs of the uncooled brain and it was also reasonably foreseeable that brain damage would arise as a result of insufficient oxygen.
Failure To Correct The Lactate Acidosis
[66] One of the indicators of oxygen deprivation is the metabolic lactate acidosis level. I find that, there were instructions to measure the lactate level. Such instructions were given obviously because knowledge of the level at various times was vital in ensuring sufficient oxygen delivery.
(See: Cross-Examination of Dr Senthi (DW 2) on page 1106 of the NOE)
"Q: My point is, Dr Lum, as an Obstetrician, was concerned about the elevated lactate levels. Are you, as an Obstetrician, concerned about it?
A: I am concerned about it but it is taken care by the Anesthetist
Q: Are you aware, can you see the abnormally high lactate levels?
A: Yes
Q: Can you see that this elevated lactate levels indicate inadequate function of the heart? Can you see that?
A: Yes
Q: Can you see that with this inadequate function of the heart, the patient's brain will not get enough supply of blood, can you see that, Doctor?
A: Can I explain...
Q: No, first of all, can you see that when there's inadequate blood supply, the heart is not functioning properly, the brain will get insufficient blood. Can you see that point?
A: Okay
[Emphasis Added]
[67] Both the plaintiff's experts have observed the level was very high for far too long as high as 7.2 mmol/L on Day No 1 before it reached the normal level at 9 am on Day No 2.
(See: paragraphs 103, 15 and 129 of Dr Lum's Expert Report on pp 67 and 70 of Bundle C)
"103. ... Lactic acidosis is characterized by a pH 7.35 and lactate level 5mmol/L.
105. Acidosis reduces cardiac contractility and cardiac output with dilation of arteries which contribute to the development of low blood pressure (hypotension)... The impaired cardiovascular function leads to inadequate oxygen supply to the tissues contributing to cardiac arrest and brain hypoxia.
129. It was only at 0900 hours on 13 December 2013, about 21 hours after YJ collapsed, that her lactate reached normal levels (Paragraph 50). As such YJ was in a chronic hypoxic state for about 21 hours which contributed to brain hypoxia (Paragraphs 105-107). Such care was sub-standard."
[Emphasis Added]
(See: Examination-in-Chief of Dr Lum (PW 7) on pp 51 and 502 of the NOE)
"Q: Do you have anything more to say about resuscitation after the initial period?
A: There are a lot of shortcomings in the resuscitation measures after the patient collapsed. I mean, the patient collapsed, they got the patient around, the follow-up was less than what it should be
Q: And what, in your opinion, was the result of those shortcomings?
A: The shortcomings contributed to the position that the patient found herself in. You had consequences for the patient, the patient had metabolic acidosis for a long period of time, which was almost 21 hours, which is a very, very long period of time
Q: These shortcomings you said led to a contribution. How substantial was that contribution to the final result?
A: Very substantial
[Emphasis Added]
(See also: Table of ABG Trends prepared by Professor Chan on pp 6 to 8 of Bundle D)
[68] It is to be noted that both medical witnesses were in an agreement that monitoring the lactel levels is important and that the normal level is around 2.0 mmol/L.
(See: Cross-Examination of Dr Adlina (DW 4) on pages 1027 to 1030 of the NOE and Cross-Examination of Dr Mohd Rohisham (DW 6) on pages 1547- 1548 of the NOE)
[69] Dr Senthi (DW 2) agreed that the low oxygenation levels will be reflected by abnormal lactate results and that obstetricians should be concerned if there are abnormal lactate levels. He also agreed that the lactate acidosis levels were abnormal.
(See: Cross-Examinations of Dr Senthi (DW 2) on pp 874 and 1104 of the NOE)
[70] Dr Adlina (DW 4) in her evidence has agreed that abnormally high lactate levels are an indication of oxygen deprivation in the body including the brain when she said as follows:
(See: Cross-Examination of Dr Adlina (DW 4) on pages 1030 to 1032 of the NOE)
"Q: You have not used the word hypoxia. I am saying, there is a connection between abnormally high lactate levels and hypoxia, insufficient oxygen delivered to the brain, do you accept that?
A: Jika Tuan merujuk kepada lactate level, tidak...
Q: It is a factor to consider?
A: Tidak specifically merujuk kepada otak sahaja, it is an indicator of a global hypo-perfusion, maksudnya tisu-tisu sel di dalam badan Puan Yusnita telah mengalami kekurangan oxygen sepertimana yang telah berlaku lah, cardiac arrest.
Q: So the tissues in the body, from head to toe, are deprived of oxygen?
A: Betul, berlaku kekurangan oxygen.
Q: Similarly, the brain, an important organ, in fact requires more than its fair share of oxygen when compared to the rest of the body, correct? Brain needs more oxygen out of proportion, the brain needs oxygen to function, correct?
A: Otak memerlukan oxygen untuk berfungsi, ya betul, saya setuju dengan pandangan Tuan.
Q: So if the lactate levels are abnormally high, that is an indication that the brain too has been deprived of oxygen?
A: Otak dan juga seluruh badan, dia tidak dapat menyatakan secara spesifik samada otak sahaja.
Q: Because we are now concerned about what had happened to her brain, right?
A: Ya, betul."
[Emphasis Added]
[71] The plaintiff's obstetric expert Dr Lum (PW 7) has testified that the lactate level should have been brought down within 2 to 3 hours and there has to be some documentation of what was done to bring down the lactate levels. However, there were no such records made in this case.
(See: Examination in Chief of Dr Lum (PW 7) on pp 57 to 509 of the NOE)
[72] The defendants' expert Dr Mohd Rohisham (DW 6) had tried to argue that the plaintiff was not hypoxic for 21 hours by relying on the measurements of oxygen saturation (SPO2) starting from the time the plaintiff had arrived in the ICU which he had said was within the acceptable range.
[73] Unfortunately, I find that he did not touch on the crucial period of 1 hour 25 minutes while the plaintiff was waiting to be transferred to the ICU without the oxygen saturation having been noted.
[74] Further, the defendants kept arguing that the oxygen concentration in the plaintiff's blood was high enough but I find that the Defendants omitted the point that the supply of blood to the brain was obviously reduced because of the bleeding. The concentration of oxygen in the blood is reflective of the amount of oxygen pumped in through the ventilator.
Premature Withdrawal Of Sedation
[75] In the instant case, I find that another act of negligence which contributed to the brain damage is the premature withdrawal of sedation as a result of which the plaintiff 'fought' the ventilator as shown in her biting the Endotracheal Tube (ETT); noticed on at least three occasions (15 December 2013, 18 December 2013 and 19 December 2013)
(See: Integrated Notes on pp 226, 260 and 269 of Bundle A1 and Cross- Examination of Dr Mohd Rohisham (DW 6) on pages 1835 to 1836 of the NOE)
[76] For ventilation to work, the plaintiff would have to be under sedation. The ETT has to be passed through the mouth into the trachea. The ETT is connected to the ventilator which provides the oxygen which is vital for maintaining body function and life. As the ETT is a foreign object, it is quite natural for the body to fight against it. I find that, the biting of the ETT caused the interruption of the flow of oxygen to the lungs and therefore the brain as well.
(See: Re-Examination of Professor Chan (PW 6) on pp 469 and 470 of the NOE)
"Q: You were referred to Bundle A1, p 226, about patient biting on tube, the SP02 you said desaturated, 93.5% of...Professor, you were asked some questions there, you said that the SP02 figure showed desaturation?
A: Yes, 93.5%
Q: Desaturation of what, oxygen?
A: Yes, that's 93.5% oxygen in the haemoglobin.
Q: Because of?
A: Because of the patient's lungs. The patient was biting on the tube, so the tube is the conduit by which oxygen moves in and the patient was not synchronizing well with the ventilator. So, at certain times, the oxygen was not moving in. Each time she opens, maybe the oxygen will go in but each time she bites on the tube, the oxygen doesn't go in. So, the gases are reflecting the poor oxygenation, if you can see, it's only 93.5% and in terms of tension, it is only 62.3 when the normal is 100 and above.
Q: Professor, what would be the normal level of SP02?
A: SP02 should be 99, 98 at least, to 100. And the P02 should be up to about 100.
Q: With this lower figures in this case, what is your conclusion regarding...?
A: The tissues are not getting enough oxygen.
Q: And with not enough oxygen, what would happen to the brain?
A: The brain would be one of the victims of this poor oxygenation."
[Emphasis Added]
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1338 of the NOE)
"Q: Now, what does sedation do in terms of she, the patient, having the endotracheal tube in her mouth?
A: It allows her to tolerate the endotracheal tube because endotracheal tube is a strong stimulus to the windpipe and also to the upper airway. And the patient may bark (sic, "buck"), may cough and that is harmful to the brain"
(See also: paragraphs 33, 34 and 38 of Professor Chan's Expert Report on p 12 of Bundle C)
[77] I find that the premature withdrawal of sedation caused the plaintiff to bite the ETT. I view that if it was necessary to withdraw sedation, it should have been done slowly and with a close observation so that she would not bite the ETT.
(See: page 8 of Bundle D; Cross-Examination of Dr Adlina (DW 4) on page 1207 of the NOE and Cross-Examination of Dr Nor'Azim (DW 5) on page 1363 of the NOE)
[78] Further, I find that the Defendants had available the option of undertaking a tracheostomy but unfortunately it was not considered or attempted early enough. This can be seen from the evidence of Professor Chan (PW 6) when she said as follows:
(See: Examination-in-Chief of Professor Chan (PW 6) on pp 268 to 270 of the NOE)
"Q: Professor, you said in the next sentence:
[PSR reads out the relevant passage(s) at p 8 of Bundle D]?
So, Professor, if re-sedation is stopped, what do they do with the ventilator?
A: What we can see here was a hurry to try to get the patient off the ventilator. But most times, providers must understand and ask themselves whether the patient is ready. Getting the patient off the ventilator, especially a patient with problems of hypoxia in the brain that has received insult in the brain, is not an easy matter. In fact, actually if we can look at the notes that is provided by the Expert from the Defence side is available, 'Mechanical Ventilation and the Injured Brain' at Bundle J. If you go to p 78, it says 'Liberation from mechanical ventilation in acute brain injury'. So, if we look at that, it accords very well with what I have been trying to say, although I must admit I never saw this article until I was provided with it because there's a general plan for patients. Anyway, the plan to liberate the patient from mechanical ventilation should be made at the initiation of ventilation. Yes, they want to hurry to get the patient out because they don't want the patient to develop other complications. But there needs to be a recognition of when mechanical ventilatory support can be reduced and ultimately discontinued.
[PWS 6 reads out the relevant passage(s) at p 78 of Bundle J]
Q: Can you stop there Professor. Having read that passage, in this case, was it one of a patient with neurological injury?
A: Yusnita had what we call brain damage or brain injury. So, whether it is meant for a trauma patient or a patient post-cardiac arrest, the brain in this particular situation had some degree of injury. So, we all treat this category of patients as a brain that is injured, that needs what we call protection. So, all our moves have to accord with this plan to protect the brain. And so, when you try to liberate or try to wean a patient from mechanical ventilation, you must take into consideration a lot of parameters that can make you lose the battle as well. So, you have to actually realize, when the patient is not ready, don't force the issue. In fact, if you look at the next page, p 79, they tell you what is the role of the tracheostomy in these types of patients. So, in fact, the tracheostomy, if done early, would have allowed the patient to have a lesser sedative requirement because remember the patient, they were trying to reduce the sedation thinking they can extubate the patient. But obviously when we are managing these types of patients with brain injury, with brain damage, we have to be very cognizant of the fact that they cannot tolerate just the tube coming out the usual way, it would be better to use a tracheostomy to come out, it's more gentle. They would have better tolerance of the weaning process, that means parting off from the ventilator, they will require less sedation. Here the patient requires it but they didn't give it to the patient because they were using a technique which was not quite appropriate to wean the patient off. They should have used a tracheostomy early enough, that's what I was also highlighting."
[Emphasis Added]
(See 1. 'Mechanical Ventilation and the Injured Brain' on p 78 of the Defendants' Supplementary Bundle of Expert Resports and Medical Literature marked as Bundle J; and
2. paragraph 3.9 of Professor Chan's Response to Dr Mohd Rohisham's (DW 6) Expert Witness Report on p 4 of Bundle D)
[79] Further, I find that the interruption of the flow of oxygen occurred at a time when the plaintiff was in dire need of oxygen. The interruption was the foreseeable result of the premature withdrawal of the sedation. This can be seen from the evidence of Dr Nor'Azim (DW 5) and Dr Mohd Rohisham (DW 6) as follows:
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1363 of the NOE)
"Q: You're explaining your answer but the reason for biting the tube was withdrawal of sedation, do you accept that?
A: I accept that"
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on pages 1620 and 1621 of the NOE)
"Q: Sometimes even, as I said a short period of poor care can cause harm. That is my point. Now Dr, each occasion, the patient bit the tube that is also a serious matter, correct?
A: It is quite often that the patient will... when they are awakening, they awaken from sedation that they will show some response including biting. They may cough, they may gag on the tube. That is considered as common. Common occurrence.
Q: But you should be mindful
A: But it they bite too long, like they said... they said they desaturate and action not taken, then yes, then it's not a good practice. But on both occasions, we have seen that the nurse actually did take action, informed the doctor and doctor did take necessary measures. That is most important. Not that you see the biting itself. Whether someone actually acted on that response from the patient, because we do see this all the time when the patient wakes up from anaesthesia, when the patient is awakening from sedation in the intensive care. This is a common occurrence.
Q: But it should be mindful, correct, of such incidence? Mindful. Would you accept that?
A: Yes."
[Emphasis Added]
[80] Dr Nor'Azim (DW 5) had given instructions to take the plaintiff on sedation on 13 December 2013 (Day No 2). On 15 December 2013 (Day No 4), the plaintiff had bitten the ETT and became desaturated.
(See: Integrated Notes on pp 199 and 226 of Bundle A1)
[81] Further evidence shows that delivery of oxygen was impeded when the plaintiff bitten the ETT on 15 December 2013 (Day No 4). The desaturation which occurred had posed an insult to the plaintiff's brain.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1354 and 1358 of the NOE)
"Q: Page 226 of Bundle A1, this is on 15th December at 12 noon, there was this entry, 'SPo2 desaturated', is that right?
A: Yes
Q: Which means that the delivery of oxygen, as measured by the pulse oximeter, was impeded, correct?
A: Yes
Q: Doctor, the fact that at p 226 of Bundle A1, it is written that there was desaturation shows that such desaturation posed an insult to her brain?
A: And it was responded to"
[82] Added to that, on 17 December 2013 (Day No 6), sedation was again taken off. On 18 December 2013 (Day No 7) the plaintiff had again bitten the ETT and became desaturated. Dr Nor'Azim (DW 5) agreed that the oxygen saturation failing to 88% was troubling and that it can cause brain damage.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1376 of the NOE)
"Q: And Doctor, when it was noted on 18th December, see p 260, 11.40am, the SPo2 has fallen to 88%. Is that troubling?
A: Yes
Q: Now, our Expert has instructed us that SPo2 should be above 95%. Those are our instructions, Doctor, do you agree?
A: I would say 88% is low, I wouldn't deny that. But whether that really has a lot of impact on the brain at that point of time, I don't think so.
Q: Doctor, when the oxygen saturation goes down to 88% as shown by pulse oximeter, it is troubling because it can cause brain damage, correct? Do you agree?
A: Yes."
[Emphasis Added]
(See also: Integrated Notes on p 260 of Bundle A1)
[83] It is to be noted that the plaintiff had for the third time bitten the tube in the early hours of 19 December 2013 (Day No 8). She was noted to have been "fighting the ventilator" and "gasping".
(See: Integrated Notes on p 269 of Bundle A1)
[84] Further, Dr Nor'Azim (DW 5) in his testimony agreed that even "5 minutes of low oxygen tension can cause harm to the brain". He agreed that an oxygen saturation rate of 88% "can cause brain damage". The defendants' anaesthetic expert Dr Mohd Rohisham (DW 6) also agreed that "short periods of say reduced delivery of oxygen to the patient would be a serious matter".
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1346, 1348, 1371 and 1379 of the NOE)
"Q: Doctor, you haven't let me finish. I will ask questions so as to put the point to you that this patient should have been managed in such a way that she would not have bitten on the tube. I will ask some question. Now, first of all Doctor, when she bit on the tube, did that affect the delivery of oxygen-enriched air to her?
A: For a short duration, yes
Q: Doctor, long or short we can debate later but it did affect her?
A: For a short duration
Q: But we do not have material, right, about these 2 events, about duration and what her observations were etc. Now Doctor, the biting on the tube can, in fact would likely result in impeding of oxygen flow into the patient's lungs, correct?
A: Yes
Q: What is the mechanical way in which that impeding of oxygen flow take place?
A: Because the passage is constricted by the biting
Q: The passage that is created by the tube, is it?
A: Yes
Q: Doctor, when the oxygen saturation goes down to 88% as shown by pulse oximeter, it is troubling because it can cause brain damage, correct? Do you agree?
A: Yes
Q: Doctor, even say, 5 minutes of low oxygen tension in the blood can cause harm to the brain?
A: Yes"
[Emphasis Added]
(See also: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1721 of the NOE)
[85] Therefore, I am of the view that if close observation showed biting of the ETT, the response by the Defendants should have been prompt so that the oxygen deprivation would be corrected without delay. However, the times when the plaintiff had desaturated and the times when measures were taken to correct the problem were not recorded.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1348, 1375 and 1379 of the NOE and Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1619 of the NOE)
[86] From the evidence produced before the Court, I am of the view that this was a case of a lapse in management. This is because no one had given evidence to testify how long the plaintiff was desaturated because nobody wrote it down what happened at the material time.
[87] Dr Nor'Azim (DW 5) had tried to defend the team by saying it had responded to the tube-biting immediately by giving Propofol but nobody could tell the Court as to whether it was actually done "immediately". I find that the amount and the timing of the giving of Propofol were not documented in the medical records or the ICU Care charts. The relevant witnesses were also not called during the trial.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1374 and 1375 of the NOE)
[88] This was further agreed by the Defendants' expert Dr Mohd Rohisham (DW 6) when he said that not enough was done as regards re-sedating the plaintiff.
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1755 of the NOE)
[89] Having perused the cause papers and the documents filed in Court, I find that there are no reliable documents to show that the Defendants had done enough. Instead, they are relying on the absence of necessary documents to defend a case that requires a "plausible explanation" at trial so as to escape a finding of negligence.
(See: Cross-Examination of Dr Nor'Azim (DW 5) on pages 1399 and 1400 of the NOE and Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1416 of the NOE)
Unnecessary Use Of PEEP And The Central Jugular Line
[90] It is to be noted that PEEP is a positive pressure applied by the ventilator at the end of each breath to improve oxygenation. Positive pressure however impedes drainage of blood from the brain which will cause cerebral oedema (swelling in the brain) and raised intracranial pressure. The result; further damage to the brain.
(See: paragraph 30 of Professor Chan's Expert Report on p 10 of Bundle C; para 3.5 of Professor Chan's Response to Dr Mohd Rohisham's Expert Witness Report on p 2 of Bundle D; Examination-in-Chief of Professor Chan (PW 6) on pp 189 to 191 and 243 to 247 of the NOE; and Cross-Examination of Professor Chan (PW 6) on pp 353 and 357 of the NOE)
[91] Professor Chan also criticized the use of a central jugular line as it also impeded cerebral venous drainage. Both PEEP and the neck line had caused the plaintiff to suffer from secondary damage to the brain.
(See: paragraph 37 of Professor Chan's (PW 6) Expert Report on pp 11 and 12 of Bundle C; and Examination-in-Chief of Professor Chan (PW 6) on pp 243 and 244 of the NOE)
[92] Dr Mohd Rohisham (DW 6) had in fact agreed with Professor Chan that PEEP can impede blood flow and should have been reduced when he said the following:
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on pages 1781 and 1785 to 1787 of the NOE)
"Q: Right, now, what is the introductory passage here at p 10 of Bundle D, 'positive and expiratory pressure PEEP, P-E-E-P, can be effective in improving oxygenation, but it may worsen or induce intracranial hypertension', which means that the brain suffers raised pressure, which is not a good thing, correct?
A: Yes.
Q: It can harm the oxygenation of the brain, correct Dr?
A: Correct.
...
Q: Should it have been reduced?
A: Reduce.
Q: It was not done.
A: I agree.
...
Q: It was unnecessary?
A: If I were there, I would have reduce.
Q: Yes, so, for the benefit of the patient?
A: Yes.
A: The reason why we taper down PEEP is not only because we feel that it may impede in the jugular, in the cerebral blood flow, but also by increasing PEEP, you can also minimise cardiac output, you can also infer on the cardiac output, blood pressure and hemodynamics monitoring"
[Emphasis Added]
[93] Further, Professor Chan (PW 6) had testified there was in fact no necessity for PEEP. The risks of PEEP outweighed the benefits.
(See: Examination-in-Chief of Professor Chan (PW 6) on p 245 of the NOE)
"Q: So he said there "During the first 15 hours", that was the PEEP range. Then he added, 'It was not necessary to kept PEEPs at this level as the oxygenation of the patient was good'. Do you agree with him, 'not necessary'?
A: That's what he said and I do agree and that's what I have been saying as well.
Q: So at least there's common ground there, Professor, PEEP was unnecessary when oxygenation was good already. You can't give too much of a good thing, Professor, I suppose that's the point.
A: That's correct"
[Emphasis Added]
Excessive Doses of Adrenaline and Noradrenaline
[94] Professor Chan (PW 6) criticized the use of noradrenaline which vasoconstricts the flow of blood and impedes the delivery of oxygen and Dr Mohd Rohisham (DW 6) agreed that such agents can impede the delivery of oxygen.
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1765 of the NOE)
[95] Professor Chan (PW 6) had described the team's use of adrenaline and noradrenaline as treating their own "medically induced problem".
(See: Examination-in-Chief of Professor Chan (PW 6) on pp 360 and 361 of the NOE)
"Q: Can you just simply take these drugs off or must be it titrated down?
A: It can be titrated down very rapidly when a patient doesn't need it. Now, one must understand that a patient who is pregnant tends to vasodilate. When a patient is pregnant, they actually vasodilate so that there's better flow to all the tissues as well as to the baby. Of course, the baby now Is not part of the equation but our blood pressure, when we are pregnant or slightly immediate post-pregnant, is never high, usually averages around 100, 110 systolic and actually the diastolic component is also not high because of the vasodilation. So, when you manage your patient, who is obstetric, no doubt she has just delivered, we do not necessarily have to treat the blood pressure until it reaches something like 120-something or whatever, just maintain it above 100 will be more than sufficient. So, what I was objecting to was using PEEP and decreasing the venous return and then treating the consequences of that because when you have decreased venous return, the cardiac output can be decreased, so the blood pressure will then drop. Then, here you are or the providers are using vasoconstrictors to try to overcome the problem they themselves have created as well as the problem the patient actually has in order to pump blood out from the heart, the patient has suffered a cardiac arrest. So, the heart and the cardiovascular system is not working as optimally as it should. So, some parts of it is actually they are treating their own, shall we say, medically induced problem. So, they have to understand, vasopressors when they are used, tend to vasoconstrict as a mechanism in order to improve the blood pressure. Yes, we do realize we have to have an adequate blood pressure to perfuse the brain but we don't just treat the blood pressure with the vasopressors agents without realizing what they are actually doing and the mechanism of action. We have to have a balance.
Q: In this case, this adrenalin were tapered off over 15 hours and this noradrenalin over 24 hours. Was this period acceptable to you?
A: We could have done it very much earlier if the providers had realized that these drugs causes vasoconstriction. When they are not needed, take it off."
[Emphasis Added]
(See also: Intensive Care Chart for 12 and 13 December 2013 on pp 14 and 15 of Bundle L)
[96] Professor Chan (PW 6) had said that adrenaline and noradrenaline could have been tapered down on Day No 2, 13 December 2013. The defendants' expert Dr Mohd Rohisham (DW 6) agreed with Professor Chan that the drugs could have been tapered down early. (See: Re-Examination of Professor Chan (PW 6) on p 465 of the NOE; Cross-Examination Dr Mohd Rohisham (DW 6) on page 1766 of the NOE)
[97] From the above, it is clear that the Defendants had failed to act on obvious facts without delay with the result that the plaintiff suffered oxygen deprivation leading to serious brain damage. Especially in the ICU, it was not enough to throw oxygen and blood at the plaintiff. Her condition had to be monitored closely. Each material changes in her condition had to act upon without delay.
[98] However, I find that the Defendants failed to do so. They allowed this to happen and failed to act without delay upon ominous signs such as biting of the ETT by the plaintiff; oxygen desaturation; and high lactate acidosis levels showing a chronic lack of oxygen.
[99] From the evidence produced during the trial, I find that the Defendants committed various acts of negligence. The severe brain damage was caused by or was materially contributed by the following factors:
99.1 the failure to undertake active cooling so as to reduce the need for oxygen;
99.2 withdrawing sedation too early, therefore causing the plaintiff to "fight" the ventilator and to bite the ETT, thereby reducing oxygen supply;
99.3 the failure to undertake an early tracheostomy so that biting or biting of the ETT could be avoided;
99.4 the unnecessary use of PEEP, resulting in impairment of arterial blood flow to the brain and impairment of cardiac output;
99.5 failing to correct the low cardiac output as shown by lactate acidosis levels beyond normal for about 21 hours, thereby causing chronic hypoxia of the brain;
99.6 inadequate documentation;
99.7 underestimation of blood loss;
99.8 to undertake transfusion of blood sufficiently and without delay;
99.9 the excessive use of adrenaline and noradrenaline, thereby impairing cerebral venous draining of blood;
99.10 consequently, raised intracranial pressure; and
99.11 the use of a jugular line.
Liability Of Expert
[100] The plaintiff brought two experts on liability, one a consultant obstetrician and gynaecologist and the other a professor of anaesthesiology. The defendants' sole expert on liability was a consultant anaesthetist in government service. Both sides brought an expert in rehabilitation medicine for the purpose of assessment of quantum.
[101] No reason was given for the Defendants' failure to call an obstetric and gynaecological expert, although there were allegations of and expert evidence of negligence in regard to the obstetric and gynaecological aspect of the case.
[102] The defendants' expert Dr Mohd Rohisham (DW 6) had said that it would have been helpful to see a suitable expert in obstetrics and gynaecology for the Defendants at trial so that the plaintiff's case could have been put to that expert.
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on page 1592 of the NOE)
[103] The other medical witnesses echoed the same sentiment with Dr Mohd Rohisham (DW 6). This can be seen from the evidence of the following doctors:
(See: Examination-in-Chief of Dr Lum (PW 7) on pp 487 and 488 of the NOE)
"Q: If I may clarify with you something Doctor, at this stage. During the time when the patient was in the OT, what role does an Obstetrician & Gynaecologist like you, would have?
A: The patient came in under the care of the Obstetrician and the Obstetrician was the one who was the primary physician, if you like, who was in charge of caring for this patient. The patient developed problems in the operating theatre, needed the assistance of the Anaesthetist to help in resuscitation. Basically, when such a situation arises, it is a team effort. But in any team, there has to be a captain, I mean football team or whatever, there is the captain and in a resuscitation team, there has also got to be a captain. And in this case, as in cases like this, the captain has to be the Obstetrician because the Obstetrician is the person who admitted the patient in the first place until the patient gets to the ICU, when the captainship is, if you like, passed over to the Anaesthetist who looks after the ICU, where they have the expertise. But that doesn't mean that in the ICU, the Obstetrician relinquishes his role, the Obstetrician still has a role to play as if there are any obstetric or surgical problems, the Obstetrician has to attend to it".
[Emphasis Added]
(See: Cross-Examination of Dr Adlina (DW 4) on pages 1212 and 1214 of the NOE)
"Q: So there should be a certain amount of cooperation between the obstetric team and the anaesthetic & ICU team, correct?
A: Betul
Q: So, if you see something which requires the attention of the obstetric team, it is your duty to inform the obstetric team?
A: Betul
Q: The other way round, if obstetric team see that there is something which the anaesthetic & ICU team should be notified of, they will tell you?
A: Betul
Q: Now, without cooperation, the patient can suffer?
A: Betul
Q: So, our Expert, Dr Milton Lum, went into matters like lactate level. Which team was looking at the lactate levels, obstetric team, anaesthetic & ICU team or both team?
A: Kedua-dua team
Q: So the obstetric team too should be concerned if they see that the lactate level is at an abnormal level?
A: Ya, betul
Q: They can tell you, they don't have to take over from you but they should tell you?
A: Ya, betul"
[Emphasis Added]
(See: Cross-Examination of Dr Nor'Azim (DW 5) on page 1248 of the NOE)
"Q: A general point, in this case, the obstetric team too was involved. Would you accept, as a general point, that the obstetric team and the ICU team should work together?
A: Yes"
[Emphasis Added]
(See: Cross-Examination of Dr Mohd Rohisham (DW 6) on pages 1519 to 1522 and 1525 of the NOE)
"Q: Doctor, in this kind of a case, when the patient was managed in the ICU, the involvement of the obstetric team was also important, would you agree?
A: Agreed?
Q: It cannot be said that all decisions in the ICU would ne made by the ICU anaesthetists or intensivists, would that be correct?
A: I agree
.......
......
Q: In fact, Dr Lum went into matters like the lactate level, do you remember?
A: Yes
Q: Now Dr Senthi, when asked about the lactate levels seen in the ICU, resisted the point that the obstetric team should be concerned about it, do you remember that?
A: Yes
Q: Do you agree with him that the obstetric team should not be concerned about lactate levels?
A: They should be concerned
....
Q: Now Doctor, you would recall, regrettably, when we were questioning Dr Senthi, he kept insisting that lactate levels were no concern of the obstetric team, I hope I got the language right. You see, don't you, that the lactate level would be a matter of concern to the obstetric team, would you accept that?
A: Yes
[Emphasis Added]
[104] However, I find that Dr Senthi (DW 2) one of the obstetricians and gynaecologists in charge, the 2nd Defendant, did not share these medical witnesses' sentiment and had insisted that the management of the lactate acidosis levels was the role of the anaesthetic team and was evasive when asked by counsel for the plaintiff about whether there should have been joint management of the plaintiff by the obstetric and anaesthetic teams
[105] I find that Dr Senthi (DW 2) kept avoiding the issues regarding the obstetric management and tried to play down the obstetric involvement in this case. I noticed that he was argumentative and trying to push the blame onto the anaesthetists, especially in regard to what had happened in the ICU.
[106] On the issue of high lactate levels, Dr Senthi (DW 2) had said that he was aware of the abnormally high lactate levels. He was also aware of the harm that the brain will suffer from low levels of oxygenation. Unfortunately, no one from the obstetric team had discussed the problem with the anaesthetic team.
(See: Cross-Examination of Dr Senthi (DW 2) on pages 116 to 1108 of the NOE)
"Q: My point is, Dr Lum, as an Obstetrician, was concerned about the elevated lactate levels. Are you, as an Obstetrician, con concerned about it?
A: I am concerned about it but it is taken care by the Anaesthetist
Q: Are you aware, can you see the abnormally high lactate levels? Can you see that?
A: Yes
Q: Can you see that this elevated lactate levels indicate inadequate function of the heart? Can you see that?
A: Yes
Q: Can you see that with this inadequate function of the heart, the patient's brain will not get enough supply of blood, can you see that, Doctor?
A: Can I explain...
Q: No, first of all, can you see that when there's inadequate blood supply, the heart is not functioning properly, the brain will get insufficient blood. Can you see that point?
A: Okay
Q: Yes, you can see that point. Inadequate supply of blood to the brain can mean that brain damage can occur, can you see that?
A: Disagree
Q: Doctor, the brain receives oxygen through the blood that is supplied to the that brain, correct, that is basic teaching, correct?
A: Okay
Q: So, if there's inadequate supply of blood to the brain, there is therefore insufficient delivery of oxygen to the brain, can you see that?
A: At what level...?
Q: Doctor, can you see that?
A: No, you are misconceived, you are misdirecting the whole perspective of the medically... how we approach these cases
Q: Doctor, are you saying that with inadequate blood supply to the brain, there would still be ...
A: Every organ in the body will suffer hypoxia ...
Q: So, when the brain suffers hypoxia, low level of oxygen, one of the results would be damage to the brain. Do you accept that Doctor?
A: I accept but I don't accept your approach, I don't accept your view. Your statement, as a general, I accept but your approach and why you're trying to pinpoint...."
[Emphasis Added]
[107] Based on the above, it is my view that the multi-disciplinary team had therefore failed in its duties and therefore its members have to collectively accept responsibility for their failure.
Causation
[108] From the evidence produced in Court, it is clear that there is an indivisible injury in this case: severe brain damage.
[109] If there appears to be more than one cause of the damage the test of material contribution to the indivisible injury would be applicable so as to establish causation to the extent of 100%.
[110] In the instant case, I view that the Defendants' negligence had at least materially contributed to the damage suffered and thus causation is proven to the extent of 100%.
[111] The plaintiff's expert in obstetrics and gynaecology, Dr Milton Lum (PW 7) said that the shortcomings in the management of this case made a very substantial contribution. Unfortunately, the defendants did not call any expert to challenge that statement.
The Experts
[112] In the instant case, I find that the plaintiff had attacked the testimony of Dr Mohd Rohisham (DW 6), the Defendants' sole expert in liability, namely the anaesthetic expert who is a government- employed doctor.
[113] According to the plaintiff, Dr Mohd Rohisham (DW 6) is not an independent expert and has failed in his duties as an expert to assist the Court. His evidence is of little assistance for the following reasons:
113.1 he was not independent, and certainly could not be seen to be independent;
113.2 he had failed to fulfill his overriding duty to the Court over any ill-conceived obligation to support his colleagues and employer;
113.3 his opinion, wherever it supported the Defendants, is based on some facts which are not proven; and
113.4 he had disregarded relevant facts or had not given sufficient weight to them.
[114] The Court of Appeal in Batu Kemas Industry Sdn Bhd v. Kerajaan Malaysia & Tenaga Malaysia Bhd [2016] 1 MLRA 36 laid down the following principles as regards the duties and responsibilities of an expert witness:
a) it is the preliminary duty of an expert to assist the Court in arriving at the right decision;
b) the duty overrides any obligation to the party from whom the expert has received instructions or by whom he is paid;
c) therefore, the evidence of an expert should not only be independent but should also be seen to be independent; and?
d) the opinions of experts are relevant only insofar as they can assist the Court in forming an opinion upon the issues in the case (s 45(1) of the Evidence Act 1950)
[115] An expert's opinion can be rejected on the ground of the lack of independence of the expert. The defendants' experts in anaesthetics and rehabilitation medicine are both employed by the Government. They were in an awkward situation no matter how hard they tried to be fair-minded. In this case, the defendants did not even call an expert in obstetrics and gynaecology although it was a case calling for teamwork between the anaesthetic and the obstetric and gynaecological teams
[116] It is my view that experts owe a duty to the cause of justice and to the Court first and only after that to the party commissioning the expert opinions. In this case, the Defendants' experts in anaesthetics and rehabilitation medicine were employees of the 17th Defendant.
[117] The defendants could have instructed experts working in public hospitals which do not come under the purview of the Ministry of Health (eg the university hospitals and the military hospitals), or even private hospitals so as to avoid any suggestion of their expert not being independent.
[118] Further, the plaintiff had experts in obstetric and gynaecology, anaesthetics and rehabilitation medicine. The defendants did not have an expert in obstetrics and gynaecology.
[119] In the present case, I find that there is no obstetric opinion, leave alone a respectable one, in support of the defendants for the Court to consider. Therefore, I view that there can be no Bolam defense.
[120] This Court finds that the Defendants have not shown that it is sufficient for an anaesthetist called by the Defendants to address the allegations of negligence and the expert evidence in support of the allegations given by the plaintiff's expert Dr Milton Lum (PW 7) who is an obstetrician and gynaecologist. In fact, I find that Dr Mohd Rohisham (DW 6) did not even address Dr Lum's expert report.
[121] At the least, the defendants should have called as an expert anaesthetic witness someone from a hospital under another ministry.
[122] However, the defendants had failed to call an obstetric expert, a fatal omission. No explanation has been given despite the averments in the Statement of Claim and the expert evidence of Dr Milton Lum (PW 7) who was the plaintiff's expert.
[123] In fact, I find that the defendants' anaesthetic expert made enough admission and concessions to help find liability against the Defendants.
Are The Defendants Liable?
[124] The Government the 17th defendant is directly liable in tort and in the contract. It is also vicariously liable for the negligence of its officers.
[125] It is also directly liable for breach of its non-delegable duty to exercise due care and skill when providing healthcare to patients so as to ensure that the healthcare provided by the staff is of a reasonable standard.
[126] The 17th defendant engaged the 1st to 16th defendants, doctors, nurses and other healthcare workers, to execute the tasks required in the provision of healthcare to patients. The 17th defendant bore the burden of designing and ensuring compliance with systems that regulated the performance of the various tasks of the individual staff members in the hospital.
[127] The fact that a member of the hospital's staff had acted negligently in breach of his or her respective individual duty to the patient does not absolve the hospital from liability. The duty to provide healthcare to the patient is a non-delegable duty and rests throughout the hospital management.
[128] In Batu Kemas Industri Sdn Bhd (supra), the Court of Appeal decided that the Government of Malaysia owed a non-delegable duty of care for work performed by an independent contractor.
[129] Even if an officer is not identified and named as a party as regards a tort, there remains the Government's liability as a contracting party which is under a duty to provide healthcare of a sufficient standard to patients. Therefore, direct liability in tort of the Government can arise because of wrongs committed by someone who was not its employee.
[130] Therefore, the Government can be found liable in tort and in the contract if the Government finds wrongs committed by a non-employee such as Dr Nor'Azim (DW 5) even though he is not a Defendant.
[131] At the least, I am of the view that the following defendants are answerable for the bad result in this case and should be held liable:
131.1 the 2nd defendant, Dr Senthi s/o N. Muthuraman;
131.2 the 3rd defendant, Dr Sureshkumar s/o Subramaniam;
131.3 the 7th defendant, Dr Noor Hetty bt Wahidon;
131.4 the 8th defendant, Dr Omar bin Sulaiman;
131.5 the 9th defendant, Dr Shazlina Shirin bt Jamaludin;
131.6 the 10th defendant, Dr Adlina bt Hisyamuddin;
131.7 the 11th defendant, Dr Tan Cheng Cheng; and
131.8 the 12th defendant, Dr Mahazir bin Kassim.
[132] The 2nd defendant, Dr Senthi was the obstetrician and gynaecologist who performed the Caesarean section. He saw the plaintiff in the ICU many times. He had seen for himself such facts in the ICU as the blood loss; the oxygen desaturation; the abnormally high lactate levels over a long period; the high temperatures; and the failure to undertake active cooling.
[133] He should have acted upon the fact the plaintiff's brain was not receiving enough oxygen. There is nothing to show that he took up the matter with the anaesthetic and intensive care team.
[134] The 10th defendant Dr Adlina, who was the medical officer on duty in the ICU on Day No 1, was the one who had first noted (at 2.45 pm on Day No 1) in the ICU that active cooling was to be undertaken.
[135] Dr Adlina had failed to act on the failure to undertake active cooling. She had failed to alert her superiors to this fact, especially when the plan was to undertake active cooling from 2.45 pm on day No 1 for 12 hours.
[136] I am of the view that the hospital management ie the government is answerable for all these failures.
[137] The 2nd, 3rd, 7th, 8th and 9th defendants had attended to the plaintiff in the Operation Theatre (OT). After the resuscitation in the OT, the plaintiff was in the recovery area of the OT unit for 1 hour and 25 minutes, waiting to be transferred to the ICU which was in another area of the hospital. I find that none of them including the nurses had written notes between 1.00 pm. and 2.25 pm. There is no documentation of the plaintiff's vital signs, such as blood loss and oxygen levels, during that period.
(See Examination-in-Chief of Dr Shazlina (DW 3) on pp 919 and 920 of the NOE)
[138] During the operation, the plaintiff collapsed, at around 11.35 am. The operation ended at 11.40 am. Resuscitation was undertaken but vital signs like the oxygen saturation were not recorded, even in the OT.
(See: Surgical Report on pp 166 and 167 of Bundle A1)
[139] Between 11.10 am. and 2.45 pm. shortly after the plaintiff was bought into the ICU, there was no record of oxygen saturation (SPO2). There is therefore a period of 2 hours and 35 minutes without this vital information having been recorded!
[140] At 2.25 pm. in the ICU the first arterial blood gas analysis (ABG) showed a predominantly metabolic acidosis picture with a lactate level which was noted as 6.0 mmol/L. It was very high, showing oxygen deprivation.
(See: 1. Intensive care Chart of 12 December 2013 on p 12 of bundle L;
2. Table of ABG Trends prepared by Professor Chan on pp 6 to 8 of Bundle D; and
3. Q & A 4 of Dr Nor'Azim's Witness Statement (DWS 5))
[141] Therefore, there was no knowledge on the part of the defendants of such vital things as blood loss and oxygen saturation during that period. The defendants' expert Dr Mohd Rohisham (DW 6) had agreed that the absence of such information during that period was a "matter for concern".
[142] In the ICU were the 10th, 11th and 12th defendants. The 10th defendant Dr Adlina wrote initial notes regarding this case.
[143] Therefore, it is clear the responsibility of the obstetric team and the anaesthetic team was to observe the plaintiff's condition in the recovery area until she arrived in the ICU when she would be handed over to the ICU team.
[144] During that critical period, at the least, the 2nd, 3rd, 7th, 8th & 9th Defendants were responsible for looking after the plaintiff. Thus, I view that they should be held liable for the omissions in the medical records.
[145] In the ICU, the 10th, 11th and 12th Defendants were responsible for looking after the plaintiff and should therefore be held liable for the adverse events that had happened in the ICU.
Conclusion
[146] In light of the above findings, the Court is satisfied that the defendants are liable for the severe brain damage as a result of severe bleeding and lack of oxygen supply to the brain of the patient following a Caesarean section performed upon her in the hospital.
[147] The Court also finds that the Government is directly liable both in tort and contract for organizational and system failures and also where it was under a non-delegable duty of care as a provider of healthcare.
[148] In light of the above, this Court finds that the plaintiff has proved its case against the Defendants on a balance of probabilities.
Quantum
[149] The plaintiff a mother of two young children suffered severe brain damage. The plaintiff is dependent on others for life. With care and treatment and facilities, the quality of her life can be improved. However, she cannot lead an independent life and earn a living and care for her family.
[150] The plaintiff has been totally dependent on others for all activities of daily living. She has no prospects of recovering much from her disabilities. However, every bit of improvement, with the assistance of care and treatment, would be meaningful.
[151] Her husband (PW 5) has been providing for the expensive care, treatment and management that the plaintiff needs.
[152] Both quantum experts Professor Lydia (PW 8) and Dr Akmal (DW 1) commended the plaintiff's husband and the other family members for taking good care of her. It is a task that requires large sums of money to be incurred. It is also physically and psychologically difficult and draining.
[153] However, despite his best efforts he does not have enough money, time, knowledge, resources and skills to provide the optimal care that the experts have recommended.
[154] She needs several carers to attend to her special needs. She also needs special medicines, therapies, appliances, equipment, a disabled-friendly environment and accommodation and special travel arrangements. The plaintiff needs care on a 24 hours basis. [See: paragraph 2.1 on p 11 of Professor Lydia's (PW 8) Expert Report on p 141 of Bundle C]
[155] The plaintiff had a fulfilling life before suffering these catastrophic injuries. Her family members have had to make various adjustments to their lives so as to care for her and her two young children.
[See: Q & A16 and 107 of the Witness Statement of Khairil Faiz bin Rahamat marked as (PWS 5)]
[156] The plaintiff's husband, sister-in-law (PW 1), mother-in-law (PW 2), mother (PW 3) and elder sister (PW 4) had testified to the hardship suffered by the entire family as a result of the plaintiff's injuries.
[157] The plaintiff's family members have been helpful. She and her family live in her parent's home in Pontian, Johor together with her elderly parents.
[158] In the plaintiff's Writ Summon, the plaintiff is claiming for.
158.1 General damages;
158.2 Interest thereon calculated at the rate of 8% per annum from the date of service of the process up to the date of judgment;
158.3 Special damages;
158.4 Interest thereon calculated at the rate of 4% per annum from 12 December 2013, up to the date of judgment;
158.5 Cost; and
158.6 Interest on the judgment sum, inclusive of general and special damages and costs, calculated at the applicable statutory rate from the date of judgment up to the date of payment.
Special damages
[159] The negligence of the defendants had caused the plaintiff to suffer serious brain damage from 12 December 2013. The claim was filed on 7 December 2015. The special damages period is therefore a period of about 23 months.
[160] Case laws are seen to suggest that credible oral evidence, in the absence of documentary evidence may be sufficient to prove special damages.
(See: Nurul Husma Muhammad Hafiz & Anor v. Kerajaan Malaysia & Ors [2015] 1 MLRH 234 Rohgetana Mayathevan v. Dr Navin Kumar & Ors And Other Appeals [2017] 3 MLRA 53)
[161] The plaintiff's husband had given evidence regarding the difficulties that he had faced in finding out if the plaintiff had a cause of action and also in keeping copies of all bills and receipts.
[162] Very often in catastrophic brain injury cases the family members of the victim are simply so overwhelmed when attending to the demanding needs of the victim that they may overlook or forget the need to keep bills and receipts for the benefit of the plaintiff.
[163] Therefore, I view that the proof of these expenses may lie in a combination of documents and the oral evidence of the plaintiff's husband.
Hospital And Medical Expenses
[164] I find that as a result of the negligence of the defendants, the plaintiff incurred hospital and medical expenses.
[165] This can be seen from the bills and invoices in support of the same which can be found on pages 1221 to 1227, 1248, 1249, 1251 to 1254 of the Common Bundle of Documents Part B Volume 5 (Bundle A5).
[166] Going by the available bills and receipts alone, the plaintiff has incurred the following sums which were paid by the plaintiff's husband and his employers
[See also: Q & A 110 to 117 of PWS 5]
[167] Even though the plaintiff's husband could not retain copies of all the bills and receipts for these expenses, I am of the considered view that this should not be a bar to the plaintiff recovering the sums incurred as pleaded. Furthermore, I find that the sum incurred is reasonable.
[168] Therefore, I allow the sum of RM27,550.80 under this item of damages.
Travelling And Accommodation Expenses
[169] It is to be noted that the plaintiff had suffered brain damage after the events on 12 December 2013 and remained in the Hospital until she was discharged home on 3 April 2014.
[170] This can be distilled from the evidence of the plaintiff's husband (PW 5) when he said that he had to travel on a daily basis from his workplace in Nusajaya, Johor to the Hospital to visit and care for the plaintiff.
Cross-Examination of PW 5 Encik Khairil Faiz on p 86 of the NOE
"A: Kalau berdasarkan pada ini, saya tak setuju lah, memang tak menyokong lah. Tapi penerangan yang saya nak sampaikan dekat sisni, sepanjang Januari sampai 2014, isteri saya masih lagi dekat wad kecemasan di bawah jagaan HSA. Tiap-tiap hari waktu bekerja, balik bekerja, saya akan menjaga dia dekat hospital, tiap-tiap hari sampai dia discaj."
[Emphasis Added]
[171] Following her discharge home in April 2014, the plaintiff's husband testified that the plaintiff had to be brought to the clinic around three to four times a month between 2014 and 2015.
Examination-in-CHief Of PW 5 Encik Khairil Faiz On Page 24 Of The NOE
"Q: En Khairil, sila rujuk ms 10, soalan 56. 'Dimanakah Yusnita dibawa untuk mendapatkan rawatan perubatan?', 'Klinik yang berdekatan'. Soalan saya En Khairil, berapa kerap Puan Yusnita memerlukan rawatan di klinik?
A: Selepas dia discharge daripada hospital, keadaan dia agak merosot, jadi kekerapan dalam masa sebulan itu mungkin dalam 3 atau 4 kali dia akan pergi klinik.
Q: Untuk berapa lama itu, kekerapan 3 hingga 4 kali sebulan tu?
A: Sepanjang 2014 sehingga 2015.
Q: Dan sekarang, apakah kekerapannya?
A: Sekarang 2 minggu sekali dia akan datang ke Klinik Desa untuk tukar... [unintelligible]..."
(See also: Q & A 56 to 58 of PWS 5)
[Emphasis Added]
[172] Following her discharge home in April 2014, the plaintiff had attended outpatient physiotherapy and occupational therapy at Hospital Pontian and speech therapy at HSA. She had also attended traditional therapy at Kulai Jaya, Ayer Hitam, Benut and Kangkar Pulai.
[173] The plaintiff was also admitted to KPJ Johor Specialist Hospital (KPJ Abd Samad) where she was admitted for around one month. During that period, the plaintiff's husband had made multiple trips to and from his workplace, his home in Kg. Rimba Terjun and had chauffeured the plaintiff's mother from her home in Sg. Durian to visit the plaintiff.
(See: Examination-in-Chief of Encik Khairil Faiz (PW 5) on pp 38 to 43 of the NOE)
[174] The plaintiff's husband had prepared a spreadsheet entitled "Travelling Record" which details the distance and frequency the plaintiff had to travel between April 2014 and October 2015. The spreadsheet does not include the travelling that the plaintiff's husband had undertaken when the plaintiff was in HSA between 12 December 2013 and April 2014 and for the times she had attended at the clinic.
(See: The Common Bundle of Documents (Part C) marked as Bundle B)
[175] Below is a table of the total travelling expenses incurred based on the spreadsheet in Bundle B.
[See also: Examination-in-Chief of Encik Khairil Faiz (PW 5) on pp 38 to 43 of the NOE]
[176] Based on the above, I award the sum of RM67,841.00 under this item of damages.
Value Of Care Provided By The Plaintiff's Family Members
[177] It is clear from the evidence given by the plaintiff's husband (PW 5), mother (PW 3), elder sister (PW 4) are her main carers and have until now been unwavering in caring for the plaintiff.
(See: 1. Witness Statement of Puan Maini binti Suliman marked as PWS 3; and
2. Witness Statement of Puan Siti Robiah binti Johari marked as PWS 4)
[178] The plaintiff's sister-in-law (PW 1) and mother-in-law (PW 2) have been involved in caring for the plaintiff.
(See: 1. Witness Statement of Puan Rashidah binti Rahamat marked as PWS 1; and
2. Witness Statement of Puan Saleha binti Hamdan marked as PWS 2)
[179] Apart from fulfilling his duties as a father, the plaintiff's husband has to:
179.1 shoulder the burden of raising their two children;
179.2 transport the plaintiff to various places for medical treatment, and also travel to stock up on her supplies and necessities;
179.3 manage his work commitments; and
179.4 ensure that the plaintiff's needs are taken care of and to supervise the plaintiff's carers.
[180] The defendants' expert on quantum Dr Akmal (DW 1) commended the plaintiff's husband and her mother (PW 3) for their dedication.
(See: Cross-Examination of Dr Akmal (DW1) on p 713 of the NOE, lines 1-12)
181. I am of the considered view that looking at the injuries suffered by the plaintiff, the plaintiff's family members have made commendable efforts to improve her quality of life. Caring for the plaintiff is no easy chore. It is laborious and taxing. Patience, dedication, perseverance and love are prerequisites.
182. In fact, the plaintiff's husband's (PW 5) overall health has taken a turn for the worse as a result of the catastrophic event in the hospital and the pressure he shoulders in caring for his disabled wife.
(See: Examination-in-Chief of En Khairil Faiz (PW 5) on pp 28-29 and 46, 61 and 76 of NOE; Q & A 106 of PW 5)
[183] Therefore, I am of the view that it is just and fair that the value of the care given to the plaintiff by the family members must be paid for by the tortfeasors. It is not right to say that, as a family, the plaintiff's relatives have an obligation to care for her. The value of such care does attract an award of damages.
(See: Tan Cheong Poh & Anor v. Teoh Ah Keow [1995] 2 MLRA 379)
[184] Considering the amount of effort and time that all of the family members have invested in caring for the plaintiff. I am of the view that the sum of RM1,000.00 per month is fair and reasonable to be awarded as the cost of care provided to the plaintiff each by her mother, elder sister and husband and RM500.00 per month to the plaintiff's brother and sister in law.
[185] Therefore, I award the cost of care provided by the plaintiff's family members as follows:
Cost Of Nutritional Supplements, Special Foods And Vitamins
[186] The plaintiff's husband had testified that he had purchased Produk Nutrilife, Elken, Honey, Enercal milk formula and multi-vitamins for the plaintiff. The receipts are found on pages 1253, 1255 to 1264, 1272 to 1283 of Bundle A5.
(See: Q & A 87 of PWS 5)
[187] He had also testified that he incurs around RM200.00 to 350.00 a month to purchase special food, nutrition and supplements for the plaintiff.
(See: 1. Q & A 89 pf PWS 5; and
2. Examination-in-Chief of Encik Khairil Faiz (PW 5) on p 26 of the NOE, lines 13-18)
[188] Based on the available documents and the testimony of the plaintiff's husband, the monthly sum of RM350.00 for nutritional supplements, special foods and vitamins during the special damages period is reasonable and should be awarded.
[189] Therefore, I award RM8,050.00 being the total cost of nutritional supplements, special foods and vitamins for the special damages period (RM350.00 x 23 months).
Cost Of Traditional Massage Therapy
[190] The plaintiff's husband had testified that he had between June 2014 and September 2015 brought the plaintiff to Kulai Jaya, Ayer Hitam, Benut and Kangkar Pulai for traditional Islamic therapy. The frequency of such therapy was three to four times a month.
(See: 1. Q & A 59 to 64 of PWS 5; and
2. Bundle B)
[191] In fact, Professor Lydia (PW 8) recognized that the plaintiff will benefit from complementary therapy. Dr Akmal (DW 1) had agreed that traditional and complementary medicine will benefit the plaintiff.
(See: 1. Paragraph 1.8 of Professor Lydia's Expert Report on p 141 of Bundle C; and
2. Cross-Examination of Dr Akmal on p 719 of the NOE)
[192] I am of the considered opinion various forms of therapy including alternative therapy for the plaintiff to bring comfort and improvement to the plaintiff and will improve her quality of life.
[193] Even though no receipts were produced following such alternative treatment by the plaintiff's husband or her family members, I find that the sum of RM600.00 is fair and reasonable.
Cost Of Diapers, Wipes And Creams And Other Personal Care Items
[194] The plaintiff's husband had testified that the plaintiff requires at least 5 diapers on a "good day' and at least 7 diapers on a "bad day". The amount of cream, wipes and other products will also increase on bad days.
[See: Q & A 96 and 97 of PWS 5]
[195] The plaintiff's husband gave evidence that he spends up to RM380.00 per month on the plaintiff's diapers, wipes and creams The pleaded sum was RM11,500.00 was given as 500.00 per month.
(See: paragraph 17.6 of the Statement of Claim on p 25 of Bundle IP)
[196] The plaintiff's husband could not provide a definite figure for these items of special damages as the plaintiff's use of these items varied from time to time. The use of such disposable items may be greater whenever the plaintiff falls sick.
[197] It is to be noted that the plaintiff is incontinent and is unable to indicate the urge to open her bowels and bladder. She needs diapers, creams, lotions and wipes to be used for her personal hygiene care.
[198] Further, I find that Professor Lydia (PW 8) had in fact estimated the cost of taking care of the plaintiff's hygiene needs, including diapers, wipes, creams, powders and etc. to be between RM500.00 and 1,000.00 per month.
(See: sub-paragraph 2.4 of Professor Lydia's Expert Report on p 142 of Bundle C)
[199] Therefore, I am of the opinion that the sum of RM500.00 per month x 23 months = RM11,500.00 is reasonable for the cost of these items
Value Of Care And Service Provided To The Plaintiff's Children And Family Previously Provided For By The Plaintiff
[200] It is to be noted that based on the evidence of the plaintiff's sister in law (PW 1), mother in law (PW 2), mother (PW 3) and elder sister (PW 4), it is clear that apart from caring the Plaintiff, they have also taken upon themselves to care for her two children which should ordinarily have been undertaken by the plaintiff if not her catastrophic injuries.
[201] In the circumstances, I view that the pleaded sum of RM32,150.00 as the value of care and services provided to the plaintiff's children is reasonable.?
Cost Of Appliances, Equipment And Special Clothing
[202] Following the Plaintiff's return home in April 2014 her husband purchased the following items which were then necessary (and are still necessary) for her care at home:
(See: 1. Q & A 95 to 99 of PWS 5; and
2. Examination-in-Chief of PW 5 Encik Khairil Faiz on pp 26 to 28 of the NOE)
[203] In the circumstances, the plaintiff should therefore be awarded the sum of RM3,377.50 for this item of damages.
Costs Of Holidays For The Plaintiff's Children
[204] The plaintiff's husband had testified that he had brought his children on holidays.
(See: Q & A 108 of PWS 5)
[205] The plaintiff's sister-in-law (PW1) has testified that she had brought the plaintiff's two children on holidays and had taken them out for walks in the park and shopping malls.
(See: Q & A 7 of PWS 1)
[206] Both Professor Lydia (PW 8) and Dr Akmal (DW 1) were emphatic in their recommendation for the provision of respite care and were of the opinion that the carers of the plaintiff need to be relieved of their duties from time to time.
[207] The stress of caring for her can be harmful to their health and can lead to disastrous consequences including the breakdown of the relationship. Such an event would be disastrous to the plaintiff, whose mother and husband are her main care providers.
[208] Therefore, I award RM600.00 under this item of damages.
Loss of Earnings
[209] The plaintiff had two sources of income. The plaintiff was an administrative executive with Mudajaya Corp Bhd Her last drawn monthly salary was RM2,150.00 in December 2013. She also sold cakes on a part-time basis.
(See: 1. Q & A 13 to 107 of PWS 5; and
2. The plaintiff's salary slips on page 1328 of Bundle A5)
[210] Based on the plaintiff's last drawn salary on December 2013, I award RM2,150.00 x 23 months = RM49,450.00 as her loss of income for the special damages period.
Cost And Expense Of Obtaining Copies Of The Medical Records
[211] It is to be noted that a successful litigant is entitled to the costs of the pre-action discovery proceedings.
[212] The plaintiff had incurred the sum of RM7,420.00 as the solicitor and client costs for obtaining copies of the medical report which were kept in the hospital.
(See: The sealed Consent Order dated 6 March 2014 in Kuala Lumpur Originating Summons No 24NCVC-123-01/2014 on pages 1350 and 1351 of Bundle A5)
[213] I view that the access to the records is a necessary step to take before bringing a claim of medical negligence. The plaintiff, his medico-legal advisers; and his experts would not have been able to give advice or opinion on the merits of this action without first having to study copies of the medical records.
[214] Therefore, I award RM7,420.00 for the costs of obtaining copies of medical records.
[215] The total award for special damages awarded is RM289,039.30.
Pre-Trial Damages
[216] The pre-trial period is from the date of filing of the claim 7 December 2015 up to the date of delivery of the decision, 15 April 2021. (a period of 63 months)
[217] It is not disputed that some of the past expenses incurred during the special damages period continued to be incurred during the pre-trial period.
Travelling Expenses
[218] The plaintiffs husband continued to incur travelling expenses during the pre-trial period of 63 months in travelling to Kg. Rimba Terjun to visit the plaintiff at her mother's home and to Pontian Town to purchase various necessities and supplies for the Plaintiff.
[219] The sum of RM300.00 per month for a period of 63 months would be reasonable for such travelling expenses. The total sum of RM18,900.00 should be allowed.
RM300.00 per month for 63 months = RM18,900.00
Cost Of Care Provided By The Plaintiff's Husband And Other Family Members
[220] Based on the injuries suffered by the plaintiff, she has continued to receive care from her husband, her elderly mother, her elder sister and in-laws.
[221] The pleaded sums for the cost of care for the special damages period should also be awarded for the pre-trial damages period. The cost of care for the pre-trial damages period is calculated as follows:
[222] The plaintiff should therefore be awarded the sum of RM220,500.00 as the cost of care provided to her over the pre-trial period.
Cost Of Nutritional Supplements, Special Foods And Vitamins
[223] The plaintiff's husband continues to purchase various nutritional supplements, special foods and vitamins for her.
[224] The sum of RM350.00 per month for a period of 63 months would be reasonable for such expenses. The total sum of RM22,050.00 should be allowed.
RM350.00 per month for 63 months = RM22,050.00
Cost Of Diapers, Wipes And Cream And Other Personal Care Items
[225] The plaintiffs husband continues to spend the sum of RM500.00 per month for the cost of diapers, wipes and creams for the pre-trial damages period. I allowed the sum of RM31,500.00 under this head of damages for the pre-trial period.
RM500.00 per month for 63 months = RM31,500.00
Value Of Care And Services Provided To The Plaintiff's Children And Family
[226] The plaintiff's eldest son was 4 years old whilst her youngest son was nearly 2 years old when the suit was filed on 7 December 2015. The plaintiff's family members continued to care for her two young children.
(See: pages 1357 and 1358 of Bundle A5)
[227] It is to be noted that as her two children grow older, they become less dependent on the plaintiff's family members. Therefore, I am of the view that the monthly sum of RM500.00 would be reasonable as the cost of care and services provided to the plaintiff's two children for the pre-trial period.
(RM500.00 per month for 63 months = RM31,500.00)
Loss Of Earnings
[228] The plaintiff continued to incur a loss of earnings in the sum of RM2,150.00 per month for a period of 63 months. The total sum of RM135,450.00 was awarded for the pre-trial period.
RM2,150.00 per month for 63 months = RM135,450.00
[229] The total award for Pre-Trial damages is RM459,900.00.
Future Damages
[230] Even though the plaintiff has managed with the care that she has received so far, her condition should not be allowed to remain in status quo.
[231] I am of the view that the plaintiff should obtain the best possible care and treatment that is available. This should not be seen as trying to seek unnecessary and unduly expensive care and treatment.
[232] The plaintiff should receive the optimal care and treatment that both Professor Lydia (PW 8) and Dr Akmal (DW 1) have recommended. Such a care regime will improve the quality of life of both the plaintiff and her carers.
[233] Therefore, it is my view that the plaintiff should be given awards of future damages for the following item:
233.1 cost of hospital admissions;
233.2 cost of medications;
233.3 cost of specialist consultations;
233.4 cost of therapies;
233.5 cost of hygiene;
233.6 cost of nutrition and supplements;
233.7 cost of assistive devices;
233.8 cost of maids and training of the carers;
233.9 value of care by his family and others;
233.10 cost of a new home;
233.11 the cost of modified vehicles; and
233.12 the additional cost of holidays.
[234] In Inas Faiqah Mohd Helmi v. Kerajaan Malaysia & Ors [2016] 1 MLRA 647, the Federal Court had decided on the standard of proof to be applied in assessing future damages which is on a balance of probabilities, but with a lower degree of certainty which can be described as a "possibility', "chance", "risk", "danger" or "likelihood".
[235] This Court would have to do the best it can in estimating the life expectancy of the plaintiff and to assess her loss post-judgment. From the life expectancy will be calculated the multiplier.
[236] The multiplier would not be relevant for past losses. It would be used to calculate the compensation for the future loss that would likely be suffered by the plaintiff so that sufficient sums of money can be awarded now and then invested to cover such loss. Unlike in England, the plaintiff cannot be awarded damages to be assessed periodically in the future. She cannot come back to Court to seek more damages for his disabilities and needs.
[237] Therefore, the Court would have to make now an award of damages once and for all basis. The Court with the assistance of the expert will have to determine her likely needs in the future and must provide for the Plaintiff by way of an award of damages now.
[238] The experts would therefore have to speculate now regarding the life expectancy, prognosis and future disabilities and needs of the plaintiff for the rest of her life. The experts will have to keep in mind the likely but not fanciful possibilities.
No Government Subsidy For Tortfeasors
[239] I am of the view that the liability of the tortfeasor should not be unreasonably and unjustifiably passed on to the public purse. Tortfeasors must not be subsidized by taxpayers. This was recognized by Tomlinson J in Maria Freeman v. Christopher Lockett [2006] Lloyd's Law Reports (Medical) 151 at 154.
[240] The healthcare services provided by the Government should not be misused for the benefit of the tortfeasors.
[241] I am of the view that if the financial consequences of the liability of a tortfeasor are passed on to the public purse, the tortfeasors (and their insurance companies, if any) would effectively be subsidized by the Government.
[242] There is no legislation compelling the Government to provide public healthcare and neither is the policy of government-funded healthcare cast in stone. Indeed, there are already public announcements of proposals to privatize healthcare in Malaysia.
[243] The plaintiff's expert on quantum Professor Lydia (PW 8) had testified regarding the challenges that patients face when seeking treatment in government hospitals. The relevant parts of her evidence are reproduced below.
Examination-In-Chief of Professor Lydia (PW 8) On Pp 65 And 606 Of The NOE
"Q: In your career, have you seen patients like these being taken to a private institution for consultations?
A: Yes, I have
Q: Why?
A: Because logistically, it is much convenient, that's No 1, No 2, the carer may be tied down with work, so they are only able to access on Saturday. So most of the public hospitals, because if it's a normal consultation, they tend not to have clinics on a Saturday. So that's why some families chose to go to private, it's basically logistic and time convenient.
Q: Professor, I have always had great regard for government hospitals and the university hospitals. What about waiting time?
A: That is also a challenge because the government hospital still have got some challenge but I know that they are trying to improve the facilities by having evening clinics and things like that. But because public hospital is meant for the public and majority of the public still access public hospital, hence there is still some moderate waiting time involved in this general case. So, some of the relatives, some of the caregivers... one of the main factor of going to a public facility is having the thought of having to wait. So, this is what bothers most of our people. So that is one of the problems of...
Court: But I thought if you have an appointment with doctor, if It's 10 o'clock, normally the waiting time will be at the most ½ hour?
A: So some facilities do try the appointment system, that means they give specific time, 10 o'clock, 12 o'clock, but it has yet to prove that it works because our public, even though the clinic starts at 10, they are still there at 8 o'clock and those who are supposed to come at 10, they come at 11 o'clock. But I think it is an improvement and it is not wrong to say that there is still some issue of waiting time. However, the government is doing their level best to try to improve it
Q: Professor, in this case of a lady with severe disabilities, how relevant is this point regarding waiting times in a busy government hospital when family members bring her there?
A: It is relevant for treatment there... in what context?
Q: I mean in terms of waiting time. If I may compare, say, with bringing a 3-year old boy who's got, say, a sprained ankle?
A: I think the importance is important, it is very important, there is no question about it because it is still alive, it is still your family member and you need to access because getting access would improve on care
Q: So Professor, given the logistics involved, bringing this lady from deep in the rural area out into a town, taking her to a busy government hospital, if there is a private hospital nearby, where everything from, say, parking to waiting time is convenient, would you say it is wrong of the family members to go to the private hospital?
A: It is not wrong, it is actually a choice of the family, whichever is convenient for... as it is, they already have a family member of this nature, so I think it is up to them. The least that we can offer to them is up to them to choose which works best for them. So, if the husband felt that it is much easier for him to access private health facilities. I think we should allow him to access private health facilities"
[Emphasis Added]
Re-Examination of Professor Lydia (PW 8) On Pp 656 And 657 Of The NOE
"Q: Now Professor, this is a matter of policy, you may not be able to answer but if patients can afford to pay, should they pay?
A: If they can afford to pay for the healthcare...
Q: I'm asking you about a matter of policy, maybe somebody from the government has to answer, but to your knowledge?
A: I think to my knowledge, healthcare should be made accessible to the whole citizen, it shouldn't be a burden to our own people. But definitely we are not able to cope with all the needs of healthcare for our population. So, there are circumstances where they do need to seek treatment in private. I don't deny that"
[Emphasis Added]
Further Cross-Examination of Professor Lydia (PW 8) On Pp 676 And 677 Of The NOE
"Q: So if you go to HRC, do HRC charge OKU person for the cost there?
A: HRC would be free, Cuma the problem is, if let's say you bring a patient like Yusnita to HRC, you will need to have a carer to be with her because HRC will not be able to provide the care needs. That is one of our limitation because we don't have enough staff. But if you were to put her in a private hospital, then they will at least not require around the clock. So sometimes a bit crazy kan, I mean you already send her to HRC but you need to have a carer, but that's one of the criteria, you can check on that. Even in our hospital in PPUM also, we would expect some level of carer but we will negotiate that you will be there for maybe 6-8 hours and then the remaining will be done by our nursing team. So, this is the limitation of our system. So, carer would expect, you hantar hospital and that's it, they can not have to stay there.
But unfortunately, that's not happening in our public hospitals, sad to say."
[Emphasis Added]
[244] The defendants' expert on quantum Dr Akmal (DW 1) who is from the government sector had acknowledged the difficulties patients face when seeking treatment at government hospitals.
Cross-Examination of Dr Akmal (DW 1) On pp 712 To 716 Of The NOE
"Q: If the patient needs assessment of rehabilitation needs and therapy and the husband finds he can come only on weekends, that will be a problem?
A: It can be a problem, yes, I agree
....
Q: Now, Doctor, spending long hours in a government hospital, whether waiting or undergoing assessment or undergoing treatment, is likely in a case like this?
A: Puan Yusnita is a disabled patient, so generally we give a priority for those who are disabled so that they don't have to wait too long compared to an able-bodied case.
Q: You will try?
A: We will try, yes, definitely
Q: But when it comes to assessment and treatment, patients like Puan Yusnita would take longer, would you agree?
A: I agree
....
Q: Doctor, my point is, have you seen that patients like Puan Yusnita have been taken to private centers?
A: Yes, I do
Q: Amongst the reasons can be time and convenience?
A: I agree
Q: Government facilities, despite all that the government provides, are, in reality, far busier than the private centers?
A: We already have the National Rehab Hospital located in Cheras
Q: My question was, they are busier?
A: Yes
Q: Waiting times can be longer?
A: Agree
....
Q: Doctor, in a rehabilitation program for the future, in a case like Puan Yusnita, is it reasonable to keep in mind private center treatment as well, consultations and management in private centers as well?
A: It's reasonable
Q: And you have seen that often enough in your cases?
A: Not quite because most of our cases they can't afford a private practice
Q: Now, of course if money is not an issue, it is something to be kept in mind?
A: Yes"
[Emphasis Added]
[245] I find that the Defendants did not bring any evidence to show that the Government will guarantee free treatment and services in terms of quality, quantity and intensity, to the plaintiff, as recommended by the experts.
[246] In fact, the plaintiff's husband had testified that the plaintiff has received poor and inadequate care and treatment from public hospitals thus far.
(See: Examination-in-Chief of Encik Khairil Faiz (PW 5) on pp 30, 31 and 47 of the NOE)?
Life Expectancy And Multiplier
[247] Multiplier is the main thing that should be fixed in determining how much general damages that should be awarded. It is appropriate to fix the multiplier in this case based on the life expectancy of the plaintiff.
[248] The plaintiff's expert Professor Lydia (PW 8) estimated life expectancy to be between 18 and 22 years from February 2017 after the second assessment undertaken by her. She added a further 3 years to that range on account of favorable economic. Dr Akmal (DW 1) had agreed with Professor Lydia's (PW 8) assessment and estimate of the plaintiff's life expectancy.
(See: Examination-in-Chief of Dr Akmal (DW 1) on p 687 of the NOE)
[249] It is to be noted that the plaintiff has so far survived for almost 7 years following the catastrophic injuries in December 2013 and according to Professor Lydia (PW 8) the fact that the plaintiff was still alive after 5 years will have a "positive" effect on her life expectancy.
(See: Examination-in-Chief of Professor Lydia (PW 8) on pp 597 and 598 of the NOE)
[250] Professor Lydia (PW 8) in her evidence on pp 587 and 592 of the NOE stated as follows:
"Q: Now Professor, if she gets good care at home, good medical care, what effect would it have on her life expectancy?
A: So, the quality of care that a patient receive is quite subjective. However, we will look at three aspects. No 1, how skilled the caregiver in taking care of the person. No 2, accessibility of the person to healthcare, that means whether the patient can be taken easily enough to access healthcare if the patient needs emergency. And No 3, if he or she has got other supportive like equipment, so there should be a standard of care that one should receive in this sort of patient. So definitely we can argue, if let's say she has got a very skill caregiver, she can be taken immediately to the hospital when she has got medical emergency, she has got all the necessary equipment to assist, it does help to improve the life expectancy of a person compared to if she does not have any of the three things that I mentioned. So that is my view. But nevertheless, quality of care still remain subjective and there are... if you look at some of the literatures over the last decade, at least the last two decades, there has been improve in the survival rate of patient in this severity, overall
....
Q: Professor, what impact on life expectancy would the items described in pp 147 and 148 have?
A: As I mentioned just now, quality of care involve 3 factors. Just to refresh, the scale, the accessibility and supporting assistive devices and equipment. So, all these will definitely improve the livelihood of the person by reducing the medical complication, improving the care to assist the carer, so that means it prevents fall, injuries, hence I would say directly that it does help to influence the life expectancy, in my opinion"
[251] Therefore, I agree with the plaintiff's submission that with the optimal care recommended by both the experts, the plaintiff is likely to do better and live longer. Therefore, I am of the view that the life expectancy should be 25 years.
Multiplier
[252] Normally deductions are made to the life expectancy when calculating the multiplier.
[253] The deductions are made for two reasons:
253.1 firstly, that the plaintiff will receive an advance payment of the damages which can be invested; and
253.2 secondly, there is a risk that the plaintiff may not reach the life expectancy estimated by the Court.
[254] In personal injury cases (excluding cases involving serious brain damage), a deduction is made from the life expectancy of an ordinary subject, as given in the national statistics. The Department of Statistics gives a life expectancy of 76 years for a Malay female.
(See: Department of Statistics Malaysia, 'Press Release Abridged Life Tables, Malaysia, 2017-2019', 23 July 2019)
[255] However, in severe brain damage cases, the life expectancy estimated by the experts would have taken into account the contingencies or the possibility of the victim dying earlier than his ordinary estimated life expectancy. Hence a reduced life expectancy estimate is made by the experts.
[256] The Courts have traditionally been expected to take into account earnings from investments and the inflation rate when deciding on the deductions to be made when calculating the multiplier.
[257] I noticed that in Malaysia, for many decades, the Courts have not reviewed or revised the discount rate. Some Courts may apply a 30% deduction whilst others may apply a 1/3 deduction irrespective of the economic conditions and the investment rate.
[258] Based on the test as set out by the Federal Court in Inas Faiqah ( supra) and the once-and-for-all basis of deciding on life expectancy. I am of the view that this Court should err on the side of awarding more instead of less.
[259] This is because if the Court errs on the side of awarding less, that will result in the Plaintiff being out-of-pocket if she survives longer than the life expectancy estimated by the Court.
[260] In Hawkins v. New Mendip Engineering Ltd [1966] 3 AUER 228, the Plaintiff suffered from temporary lobe epilepsy and was at risk of developing major epilepsy sometime in the future. The trial judge awarded substantial damages including for the cost of treating any future major epilepsy. The award for damages was upheld on appeal by the Court of Appeal Judges approving the benefit of the doubt that the trial judge had given to the plaintiff. The relevant parts of the judgment of the Court of Appeal in Hawkins (supra) are quoted below:
Wilmer L.J. on p 229:
The problem in this case is to forecast what is likely to happen in the future. For it has now transpired as the result of medical examination, and as a result of the analysis by doctors of certain symptoms which this young man subsequently developed, that he is at present suffering from what is called temporal lobe epilepsy. That is, as I understand it, a relatively minor form of epilepsy, but there is a risk (and a serious risk) that at some time in the future, necessarily an uncertain future time, this young man may develop major epilepsy. If he did so, of course, it would necessarily alter the whole tenor of his life. It might affect his ability to earn his living, at any rate in doing any such job as be is doing at present and inevitably it would grievously affect his social and domestic life and everything that goes to make up the amenities of life. The doctors in their evidence were unanimously of the view that in a case of this sort it is virtually impossible to tell within the first five years of the accident what the future is likely to be. The position, therefore, was that the learned judge had the difficult, and one might say the almost impossible, task of putting into pounds, shillings and pence what might be the effect of a wholly uncertain future. That is the result of our procedure, which requires the Court to award a sum of damages now, once and for all, which is sufficient to take care of likely future possibilities. It was in those circumstances that the learned judge came to award this very considerable sum of £8,000 for general damages.
Winn L.J. on p 232:
"I agree, and I agree with the reasoning of Wilmer LJ's judgment. In my opinion, if the leaned judge had awarded any appreciably smaller sum in this case, he would have been taking an unjustifiable gamble with the future of this young man."
Scarman J on p 233:
"I agree. This case is a very good illustration of the impossibility of the task which sometimes faces a judge in the assessment of damages. In this case the trial judge was called on to make his once-for-all assessment of damages at a time when, according to the medical evidence, it was quite impossible to make a prognosis of the future even on a balance of the probabilities. The distinguished neurologist who gave evidence, Dr Gordon Campbell, when asked what he would say if required to give a prognosis, replied in these terms:
"I should have thought that he [the plaintiff] would undoubtedly have to be watched and treated for five years, and that one would not be able to give a satisfactory answer as to his future until that time had elapsed."
Yet the trial judge had to give an answer, satisfactory or otherwise, to that particular problem. It is not surprising, therefore, that at an early stage in his judgment the judge said: "Whatever figure I decide on will on any view be guesswork, and my guess is as good or as bad as anybody else's." I respectfully agree with the learned judge, and for that reason I agree also that this appeal must fail."
[Emphasis Added]
[261] I find that Hawkins (supra) was approvingly referred to by the Federal Court in Inas Faiqah (supra) and by the High Court in Farah Ahmed Naji Al Sahhaf v. Dr Lee Weng Seng & Ors [2017] MLRHU 1761.
[262] Further, in James Robshaw (A Child by His Mother And Litigation Friend, Suzanne Adams [2015] Med LR; [2015] EWHC 923(QB), the Court added 3 years to the life expectancy on the ground that the damages award would result in better care, treatment, facilities etc. for the Plaintiff and therefore a longer life expectancy.
[263] In the circumstances and going by the guidance in Hawkins (supra) and Inas Faiqah (supra) I am of the considered view that the plaintiff should be given the benefit of the doubt and the life expectancy should be given as 25 years, taking the 22 years estimated by Professor Lydia and agree to by Dr Akmal, with an additional 3 years on account of favorable economics.
Multiplier
[264] Therefore, based on the above, the multiplier to be applied in this case should be the additional 25 years of life expectancy less the 3 years she has survived so far and less a further 15% for the contingencies and vicissitudes of life.
Future Needs Of The Plaintiff
[265] It is to be noted that this Court has to rely on the expert evidence in assessing the future needs of the plaintiff.
[266] Professor Lydia (PW 8) and Dr Akmal (DW1) had each given a fairly exhaustive list of equipment, appliances, medicines, medical supplies, and nutrition that the plaintiff will require now and in the future.
(See: 1. Appendices 1 and 2 of Professor Lydia's Expert Report on pp 145 and 146 of the Bundle of Expert Reports marked as Bundle C]
2. Tables of Dr Akmal's recommendations on pp 162 to 164 of Bundle C]
[267] I find that there were some items on which there was disagreement between them regarding the cost and some items where there was disagreement as regards the need for them.
[268] It is to be noted that the plaintiff has a duty to mitigate her losses. However, I am of the view that the plaintiff should not suffer a sacrifice of her well-being and the welfare of her carers.
[269] I find that the experts have given their opinions regarding the therapeutic benefits of their respective recommendations. Therefore, I view that the benefit should be the main consideration when awarding the cost of purchasing such equipment. Given her debilitating condition, I am of the considered opinion that the plaintiff should be given every reasonable advantage possible. It will be an 'unjustifiable gamble' for the plaintiff to not be awarded the cost of such equipment, medicine and therapies.
Cost Of Assistive Equipment And Other Items - Disputed Items
(i) Alternating Pressure Mattress
[270] Professor Lydia (PW 8) had recommended the provision of an alternating pressure mattress to reduce the need for her mother (PW 3) to have to wake up at night to turn the plaintiff at intervals.
(See: Item 2 of Appendix 2 of Professor Lydia's Expert Report on p 146 of Bundle C)
[271] Dr Akmal (DW 1) recognized that such a task can be taxing on the plaintiff's mother. Dr Akmal did not think that Professor Lydia's recommendation for an alternating pressure mattress was unreasonable.
(See: Cross-Examination of Dr Akmal (DW 1) on pp 730 to 732 of the NOE)
[272] Dr Akmal's contention in support of her recommendation for a ripple mattress which she had called the "lower-end" mattress has the same function as the alternating pressure mattress and that it was just a "matter of quality".
(See: Cross-Examination of Dr Akmal (DW 1) on p 732 of the NOE, lines 4 -16)
[273] In the circumstances, I am of the view that the plaintiff should be awarded the sum of RM24,000.00 being the cost of purchasing an alternating pressure mattress as recommended by Professor Lydia with two replacements over the life expectancy period of 25 years.
RM8,000.00 x 3 units = RM24,000.00
(ii) Tilt-In Space Wheelchair And Recliner Wheelchair
[274] Professor Lydia (PW 8) recommended the provision of a tilt in space wheelchair with head support and body straps to allow for transportation, stimulation and for sitting and pressure relief.
(See: Item 3 of Appendix 2 of Professor Lydia's Expert Report on p 146 of Bundle C)
[275] Dr Akmal (DW 1) had for the same purpose as Professor Lydia recommended the semi light-weight recliner wheelchair size 16 inches with a detachable arm and foot rest together with a wheelchair cushion size 16x16 inches.
(See: Item 1 of the list of required assistive devices on p 163 of Bundle C)
[276] Professor Lydia had agreed that the plaintiff will need both her and Dr Akmal's recommended wheelchairs.
Cross-Examination of Professor Lydia On P 639 Of The NOE
"Q: Only item No 3 is sufficient for this patient, at p 146 of...?
A: Yes. However, if let's say the patient needs to go out for recreational, that means the husband wants to take her to another family's house, to bring a Tilt-in-Space, it is quite a bulky wheelchair, we acknowledge that. So, it is quite reasonable for them to have another wheelchair like what Dr Akmal suggested, which is more portable. This is just basically portability where else the one that I suggested is a good seating system that she can use at home for a longer time. But you do not want to have the trouble to bring it all in a car, especially if you have got a sedan car, you don't have the space, it is quite troublesome. So usually people will have few wheelchairs because one will be small enough and easy enough for them to put in the car because nobody likes to bring along a very bulky item. So that is the answer".
Re-Examination of Professor Lydia (PW 8) On P 667 Of The NOE
"Q: Do you have any views about this bulky Tilt-in Wheelchair and shall I say, ordinary smaller wheelchair. Do you have any views about having both for that patient?
A: Yes
Q: What is your view?
A: You would need both"
[Emphasis Added]
[277] Based on the above, I award the plaintiff as follows:
a) Tilt-in space wheelchair with head support and body straps - RM10,000.00.
b) Semi light weight recliner wheelchair size 16 inches with detachable arm and foot rest and wheelchair cushion size 16 x 16 inches - RM5,320.00.
Tilt Table With Tabletop
[278] Professor Lydia (PW 8) recommended for the provision of a tilt table for its therapeutic benefit in terms of standing therapy.
(See: Examination-in-Chief of Professor Lydia (PW 8) on p 591 of the NOE; Item 14 of Appendix 2 of Professor Lydia's Expert Report on p 146 of Bundle C)
[279] Professor Lydia (PW 8) had also given reasons why the tilt table is a more suitable option for the plaintiff compared to the manual standing frame which was recommended by Dr Akmal (DW 1). (See: Cross-Examination of Professor Lydia (PW 8) on pp 640 and 641 of the NOE)
[280] In the circumstances, I award the sum of RM10,000.00 being the cost of purchasing the tilt table.
(iii) Shower Trolley
[281] Professor Lydia (PW 8) had recommended the provision of a shower trolley in the event the plaintiff is unable to sit up or when her posture is compromised due to spasticity. If the spasticity is not adequately and appropriately managed, there will be a need for the shower trolley in addition to the commode chair.
(See: Cross-Examination of Professor Lydia (PW 8) on p 643 of the NOE; item 6 of Appendix 2 of Professor Lydia's Expert Report on p 146 of Bundle C)
[282] Dr Akmal (DW 1) had said that she will not reject professor Lydia's recommendation for a shower trolley.
Cross-Examination of Dr Akmal (DW 1) On P 736 Of The NOE
"Q: Given that Professor Lydia has recommended a shower trolley for use in the future, can that recommendation be rejected on scientific grounds or medical grounds?
A: No".
[283] Going by the guidance and advice in Inas Faiqah (supra) and Hawkins (supra), I am of the view that the plaintiff should be awarded the sum of RM30,000.00 being the cost of purchasing the shower trolley with two replacements over the life expectancy period of 25 years.
RM10,000.00 x 3 units = RM30,000.00
Pulse Oximeter With Alam Digital Blood Pressure Machine, Digital Ear Thermometer And Glucometer Set (Monitoring Devices)
[284] On this issue, I agree with the defendants' submission that the types of equipment are not needed as they are merely monitoring devices and the plaintiff is not put at high risk at diabetes in the future.
[285] The plaintiff, as well as any other person in general are mutually at risk to develop diabetes and this does not mean every other person must purchase the equipment mentioned above and thus, there is no necessity for the plaintiff to claim for the equipment mentioned above.
Sensory Stimulation Kit
[286] Dr Akmal (DW 1) testified that the sensory stimulation kit can be found in hospitals and can be carried out by medical practitioners in hospitals. Looking at the condition of the plaintiff that has plateaued over the span of 5 years. Since there has been no noticeable improvement in brain consciousness, thus it would suffice that the process of sensory stimulation is conducted by medical practitioners at the hospital.
(See: Examination-in-Chief of Dr Akmal (DW 1) on pp 695-696)
[287] I find that the price of RM5,000.00 for a sensory stimulation kit is an equipment that has been designed commercially. It is expensive because it is not designed locally. Therefore, I view that there is no necessity for the plaintiff to have this equipment and it also comes at a hefty price. It will definitely not aid in recovering or improving the plaintiff's brain consciousness as it has plateaued over the past 5 years.
Renovation Of The Home
[288] In her expert report, Professor Lydia (PW 8) made the following recommendations for the Plaintiff's proposed home environment:
288.1 that there should be adequate access to the bathroom to allow for daily baths;
288.2 that the home should have adequate space for the undertaking of home-based rehabilitation; and
288.3 that the home should have one room with an attached toilet for activities such as nursing and toileting in privacy.
(See: 1. page 142 of Bundle C; and
2. Examination-in-Chief of Professor Lydia on pp 619 to 622 of the NOE)
[289] The plaintiff stays in her parents' single-storey house which has two bedrooms and one bathroom. She is placed on a mattress in the living area of the house. The bathroom is small and is not able to accommodate a commode chair.
(See: 1. page 142 of Bundle C; and
2. page 159 of Bundle C)
[290] Dr Akmal (DW 1) could not comment on the inadequacy of the plaintiff's current home. She has not visited the house nor did she view any pictures of the house.
(See: Cross-Examination of Dr Akmal (DW 1) on pp 761 and 762 of the NOE)
[291] It was never suggested to the experts by the learned Senior Federal Counsel that home modifications were not necessary in this case. Further, I find that the Defendants did not bring evidence of the cost of home modifications.
[292] In the circumstances, I am of the considered view that the plaintiff should be awarded the sum of RM100,000.00 being Professor Lydia's estimated cost of home modifications.
(See: page 143 of Bundle C)
[293] However, I am of the view that a one-half deduction be made to the cost of renovations of the plaintiff's current home as calculated below:
the cost of renovations = RM100,000.00
minus half for benefit of others = (RM50,000.00)
total = RM50,000.00
Cost Of Medical, Therapy And Other Services
(i) Medical Consultations And Therapies
[294] On this issue, I find that both experts did not disagree with one another's views regarding their recommended medical consultations and therapies.
[295] Professor Lydia (PW 8) had opined in her expert report that the plaintiff may require short-term acute hospital admissions and also admissions for intercurrent illness or planned procedures. She has opined that the visits to the hospitals and/or clinics will be due for the following reasons:
295.1 respiratory issues such as aspiration, orthostatic pneumonia and respiratory tract infection;?
295.2 gastrointestinal issues arising from issues with the nasogastric tube, insufficient nutrition and gastrointestinal tract disturbance;
295.3 multi-organ failure;
295.4 insertion of the percutaneous endoscopic gastrotomy (PEG) tube; and
295.5 dental consultation.
(See: Professor Lydia's Expert Report on pp 138 and 139 of Bundle C)
[296] In the circumstances, Professor Lydia (PW 8) had estimated the frequency of hospital admissions to be an average of 3 to 4 times a year. Dr Akmal (DW 1) did not disagree with Professor Lydia or provide a different view.
[297] Professor Lydia (PW 8) also did not disagree with Dr Akmal's recommendations for consultation with a neurologist and speech therapy.
[298] Dr Akmal testified that the plaintiff suffers from contractures and will require surgery for contracture release which costs around RM4,000.00.
(See: Cross-Examination of Dr Akmal (DW 1) on pp 742 and 743 of the NOE)
[299] Dr Akmal (DW 1) testified that the plaintiff may require admission to the hospital for intravenous antibiotics due to respiratory infection. She had estimated the frequency of these admissions to be twice a year and the cost would be around RM3.000 per admission.
(See: Cross-Examination of Dr Akmal (DW 1) on pp 754 and 755 of the NOE)
[300] Based on Inas Faiqah (supra) and Hawkins (supra), I am of the view that the plaintiff should be awarded the cost of all the medical consultations and therapies recommended by both experts. I award the sum of RM19,000.00.
[301] Professor Lydia (PW 8) had recommended the provision for the cost of ambulance services in the event, the plaintiff requires admission such as when she develops deep vein thrombosis in her leg or severe respiratory distress due to aspiration pneumonia. Professor Lydia (PW 8) had estimated the cost of such services to be RM200.00 per trip which services may be required 6 to 8 times a year.
(See: 1. Item 6 of Appendix 1 of Professor Lydia's Expert Report on p 145 of Bundle C; and
2. Cross-Examination of Professor Lydia (PW 8) on p 608 of the NOE, lines 11 -19)
[302] Although Professor Lydia (PW 8) had said in her expert report that an ambulance will not be required as often if the adapted vehicle is available, she had testified that in the event the plaintiff is unable to tolerate sitting too long, it would be better for her to lie down on a stretcher in which case an ambulance would be a more suitable option.
(See: Cross-Examination of Professor Lydia (PW 8) on p 654 of the NOE, lines 15-22)
[303] Professor Lydia (PW 8) had also testified that the plaintiff may require an ambulance if and when the plaintiff's husband is not around to drive her to the hospital or the clinic.
(See: Cross-Examination of Professor Lydia (PW 8) on p 655 of the NOE, lines 5-11)
[304] In the circumstances, I award the plaintiff the sum of RM30,400.00 being the cost of ambulance services 8 times a year.
(RM200.00 per trip 8 times a year x 19 = RM30,400.00)
(iii) Cost Of Required Medication
[305] The plaintiff also claimed the cost of required medication and I allow the claim as follows:
List Of Requires Medication
Value Of Care
[306] It is not disputed that the plaintiff's mother and her husband continue to be her main carers. They will have to continue to manage and supervise the provision of care, treatment and nutrition to the Plaintiff.
[307] Certainly, the benefits of having the carers, equipment and therapist as recommended by the experts will reduce the Plaintiff's husband's and mother's burden but will not alleviate it completely. They will still need to supervise her carers and the Plaintiff's husband will still need to manage the purchase of her supplies and necessities.
[308] Therefore, I view that the sum of RM1,000.00 per month should be awarded as the total value of care provided by the plaintiff's husband, mother and other family members.
RM1,000.00 per month for 19 years = RM228,000.00
(RM1,000.00 x 12 x 19 = RM228,000.00)
Future Loss Of Earnings
[309] The plaintiff's last drawn salary was RM2,150.00 per month in December 2013. Going by s 28 of the Civil Law Act 1956, the Plaintiffs loss of earnings is to be calculated as follows:
55 years minus 40 years = 15 years
15 divided by 2 = 7.5 - multiplier of 8
RM2,150.00 x 12 for 8 = RM206,400.00
Pain And Suffering And Loss Of Amenities Of Life
[310] The current trend of awards may give the Court guidance in determining the amount of damages for pain and suffering.
[311] I noticed that the awards for a victim of a tort suffering from brain damage in recent cases have been between RM 385,000.00 and 500,000.00.
[312] In Henry Siang Len v. Universiti Kebangsaan Malaysia & 17 Ors in Kuala Lumpur High Court Suit No WA-22NCVC-795-12/2016 (Unreported), Mohd Zaki Wahab J had awarded RM500,000.00 as general damages for pain and suffering and loss of the amenities of life to the Plaintiff who was a brain-damaged adult in a persistent vegetative state. The award was not disturbed in the Court of Appeal.
[313] In Fareed Reezal Arund (Mendakwa Melalui Isteri Dan Wakil Litigasinya, Wan Zafura bt Wan Kassim) lwn. Pantai Medical Centre Sdn Bhd dan Yang Lain (KL High Court Suit No WA-22NCVC-33-01/2016) (unreported). Wan Ahmad Farid J had awarded the sum of RM400,000.00 as general damages for pain and suffering and loss of amenities of life to the Plaintiff who is also a brain-damaged adult.
[314] In Piona Abdul Latif v. Kerajaan Malaysia & Ors [2018] MLRHU 527 which is another case involving a brain-damaged adult, the learned Judge had awarded the sum of RM800,000.00 as general damages for pain and suffering and loss of amenities of life which were later reduced to the sum of RM400,000.00 by the Court of Appeal.
[315] In the following brain damage cases, the awards for pain and suffering and loss of amenities of life were:
315.1 RM385,000.00 in Rohgetana Mayathevan v. Dr Navin Kumar & Ors And other Appeals [2017] 3 MLRA 53; which sum was upheld by the Court of Appeal;
315.2 RM400,000.00 in Muhammad Yassien bin Zuliskandar (Seorang Kanak-Kanak Yang Mendakwa Melalui Bapanya Dan Sahabat Wakilnya Zuliskandar b Md Peckor) & Ors v. Kerajaan Malaysia [2010] 13 MLRH 748;
315.3 RM400,000.00 in Farah Ahmed Naji Al Sahhaf (supra) which sum was upheld by the Court of Appeal;
315.4 RM400,000.00 in Harraz bin Abdul Halim & Anor v. Dr Azlina Abdul Aziz & Ors [2018] MLRHU 1060 which sum was upheld by the Court of Appeal; and
315.5 RM400,000.00 in Fazli Suboh & Ors v. Dr Fatimah Ahmad Fauzi, Guaman Sivil: MTKL 21NCVC-88- 12/2015.
[316] Unlike infants who suffer brain damage at birth, the plaintiff herein has had an appreciation of the joys of life, childhood, marriage, motherhood, successful vocation and etc. The negligence of the defendants has deprived her of all these joys. Her loss of amenities of life is therefore far more than infants who had suffered brain damage at birth.
[317] In the circumstances, I award the sum of RM400,000.00 under this head of damages.
Costs
[318] It is a well-recognized fact that medical negligence litigation is very expensive. The legal costs in a medical negligence claim can be considerable, compared to the value of the claim. Medical negligence litigation is difficult, complex, time-consuming and often involves novel questions of law and fact.
[319] Alec Samuel said in The English Tort System for Medical Mishaps', Medico- Legal Journal (2004) Vo 72, Part 4, p 147.
"Costs often exceed the compensation and comparatively few patients end up with compensation...'
[320] The editors of Powers and Harris on Clinical Negligence (4th Ed) say in para 11.4:
"Legal costs particularly in clinical negligence litigation, can be considerable compared to the value of claims".
[321] The editor of Charles J Lewis on Medical Negligence - A Plaintiff's Guide (2nd Ed) says on p 39:
"Medical negligence actions are very expensive."
[322] In Farah Ahmed Naji Al Sahhab (supra), Nantha Balan J (now JCA) awarded the sum of RM250,000.00 as a getting-up fee for both the liability and quantum proceedings involving a brain-damaged infant. The defendants admitted liability well before the trial.
Getting Up Fee: Liability And Quantum
[323] The suit was filed on 7 December 2015 in the High Court at Kuala Lumpur. The trial commenced after almost two years as the Defendants had applied for the proceedings to be transferred to Johor Bahru.
[324] The trial proceeded for 23 days over a period of almost three years from 10 July 2017.
[325] A total of 14 witnesses testified. The majority of the witnesses were medical and expert witnesses.
[326] The following sub-specialties of medicine were involved in the case:
326.1 obstetrics;
326.2 anaesthesiology; and
326.3 rehabilitation medicine.
[327] Going by the complexity and novelty of the issues involved, I am of the view that the sum of RM250,000.00 should be awarded as the getting-up fee for the liability and quantum proceedings.
[328] I also allow the out of pocket expenses in the sum of RM104,682.47 in full.
(See: Annexure 4 in the Plaintiff's written submission (Enclosure 54))
Conclusion
[329] A summary of the Award of this Court as mentioned above is reflected in the table below:
Special Damages
Pre-Trial Damages
General Damages For Pain & Suffering And Loss Of Amenities Of Life
Life Expectancy And The Multiplier
Future General Damages
Costs
Interest
Summary